Nose-picking Healthcare Workers Were More Likely to Get COVID

A study of healthcare workers (HCW) found that those who picked their nose were more likely to get COVID than the people who refrained from such explorations. The Dutch researchers published their probing results in the journal PLOS One.
In the early stages of the COVID pandemic, researchers noted a wide range of efforts to prevent the spread of SARS-CoV-2, such as the wearing of personal protective equipment and maintaining social distancing, especially in the hospital setting. Much research went into the impacts of, eg, wearing glasses on the effectiveness of masking, but little if any attention was paid to a widespread but secretive habit.
Sikkens and colleagues retrospectively surveyed healthcare workers at Amsterdam University Medical Centers were in December 2021 about their behaviours during the first and second waves of the pandemic. They matched these responses were matched against prospectively collected COVID test results at the hospitals from March to October 2020. The nose pickers were nearly three times more likely to catch COVID (17.3% vs 5.9%) than those who refrained at all costs. Surprising results were found for those HCWs who owned up to the habit.
Secret nose pickers can take some comfort in that 85% of the cohort admitted that they picked their nose either daily, weekly, or monthly, and nose pickers tended to be younger. More men picked their nose (90%) than women (83%), and doctors were the most likely to be among the nose-picking offenders: 100% of residents admitted to it, along with 91% of specialists.
Sikkens et al. noted that one limitation of the study was that nose pickers were not asked about “the depth of penetration and eating of boogers”.
Other behaviours such nail biting, having a beard were not associated with COVID infection, nor was wearing glasses, though it showed a relevant trend. Interestingly, nose picking frequency was not linked to difference in COVID infection risk; 27% of those who reported monthly picking, 35% among weekly pickers, and 32% of daily pickers.
Frequency of nose picking did not appear to be linked with any difference in COVID infection risk, with positive cases in 27% of those who reported monthly picking, 35% among weekly pickers, and 32% of daily pickers. No participants reported picking their nose every hour, thankfully.
One-third of the cohort reported nail biting, two-thirds wore glasses, and 31% of the men had beards.
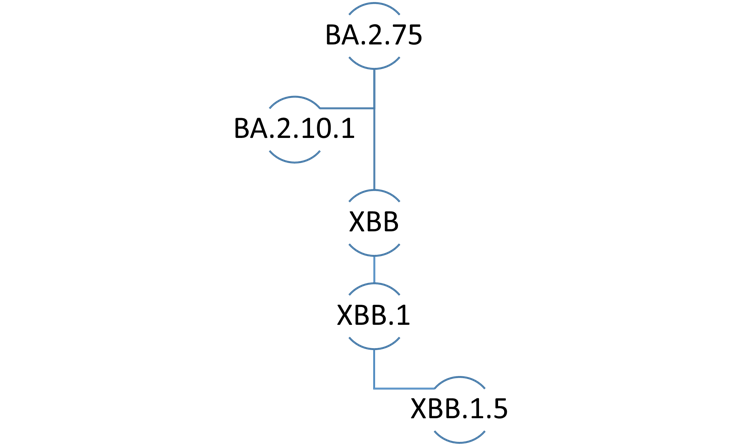
A study strength was that SARS-CoV-2 positivity was determined by prospective longitudinal serological sampling, though this may not be generalisable to the current era of vaccines and circulating Omicron variants. The retrospective nature of the survey may have introduced recall bias.
Sikken et al. noted that it is surprising that SARS-CoV-2 transmission routes had been so thoroughly researched, yet simple behaviours had been overlooked. “Possibly this sensitive subject is still taboo in the health care profession. It is commendable we assume HCWs to not portray bad habits, yet we too are only human after all, as illustrated by the pivotal proportion of nose pickers in our cohort (84.5%).”