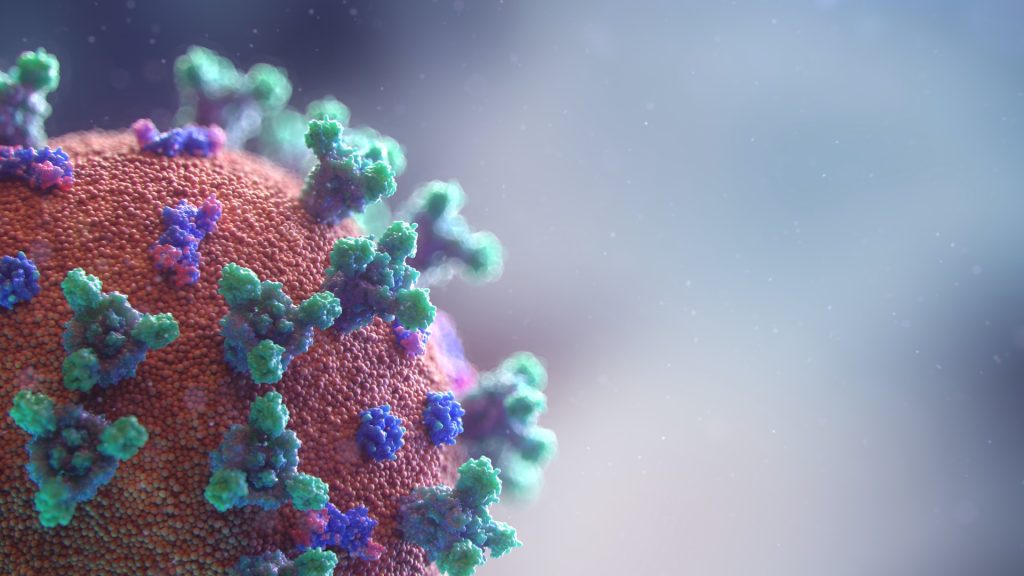
Rapid Blood Assay to Test for COVID Immunity

Researchers have developed a rapid blood assay that measures the strength and duration of an individual’s immunity to SARS-CoV-2. This test will allow population-scale monitoring immunity and vaccine effectiveness. This will help to design revaccination strategies for vulnerable immunosuppressed individuals, according to a study published by the researchers from Mount Sinai in Nature Biotechnology.
The test, which measures the activation of T cells, is performed in under 24 hours and can be scaled up significantly.
“The assay we have created has the ability to measure the population’s cellular immunity and broadly test the efficacy of novel vaccines,” said one of the study’s senior authors, Ernesto Guccione, PhD, Professor at Mount Sinai. “We know that vulnerable populations don’t always mount an antibody response, so measuring T cell activation is critical to assess the full extent of a person’s immunity. Additionally, the emergence of SARS-CoV-2 variants like Omicron, which evade most of the neutralising ability of antibodies, points to the need for assays that can measure T cells, which are more effective against emerging variants of concern.”
Long-term protection from viral infection is mediated by both antibodies and T cell response. Many recent studies point to the importance of determining T cell function in individuals who have recovered from or been vaccinated against COVID to help design vaccination campaigns. However, before this study, measurement of T cell responses has been rarely performed because of the associated technical challenges.
Researchers optimised qPCR-based assays that had the potential to be globally scalable, sensitive, and accurate tests. They then selected the two assays that offered the most scalability. One, the qTACT assay, was accurate and sensitive but had a relatively longer processing time of 24 hours per 200 blood samples, a moderate price, and a medium level of technical skill. The other, the dqTACT assay, was accurate and had a reduced processing time and cost, and required minimal lab experience, making it easy to implement.
The dqTACT assay has recently received the European CE-IVD (in vitro diagnostics) certification, while U.S. Food and Drug Administration and European Medicines Agency clinical validation is ongoing.
“The assays presented here are based on the ability of SARS-CoV-2 T cells to respond to peptides covering different proteins of the virus,” said another senior author, Jordi Ochando, PhD, Assistant Professor at Mount Sinai. “With the possibility of using different peptide pools, our approach represents a flexible strategy that can be easily implemented to detect the presence of T cells responding to different viral proteins. These T cells have an important role in protection from emerging mutant strains, thus immediately gauging the impact that viral mutations might have on cellular immunity.”
Megan Schwarz, a graduate student at Icahn Mount Sinai and first author of the study, added: “Precise measurement of cellular responses underlying virus protection represents a crucial parameter of our levels of immune defence.”
Source: EurekAlert!