Specific Nasal Cells Protect against COVID in Children
Important differences in how the nasal cells of young and elderly people respond to the SARS-CoV-2 virus, could explain why children typically experience milder COVID symptoms, finds a new study led by researchers at UCL and the Wellcome Sanger Institute.
The study, published in Nature Microbiology, focused on the early effects of SARS-CoV-2 infection on the cells first targeted by the viruses, the human nasal epithelial cells (NECs).
These cells were donated from healthy participants, including children (0–11 years), adults (30–50 years) and, for the first time, the elderly (over 70 years).
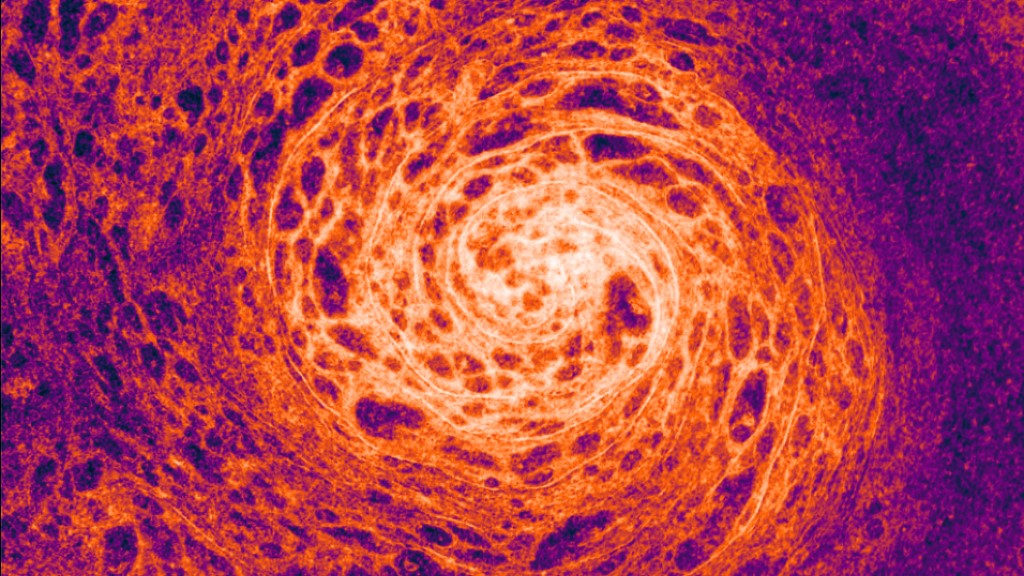
The cells were then cultured to regrow into the different types of nasal cells. Using single-cell RNA sequencing techniques that enable scientists to identify the unique genetic networks and functions of thousands of individual cells, the team identified 24 distinct epithelial cell types. Cultures from each age group were then either mock-infected or infected with SARS-CoV-2.
After three days, the NECs of children responded quickly to SARS-CoV-2 by increasing interferon (the first line of anti-viral defence), restricting viral replication. However, this early anti-viral effect became less pronounced with age.
The researchers also found that NECs from elderly individuals not only produced more infectious virus particles, but also experienced increased cell shedding and damage.
The strong antiviral response in the NECs of children could explain why younger people typically experience milder symptoms. In contrast, the increased damage and higher viral replication found in NECs from elderly individuals could be linked to the greater severity of disease observed in older adults.
Project lead, Dr Claire Smith (Associate Professor at UCL Great Ormond Street Institute of Child Health), said: “Our research reveals how the type of cells we have in our nose changes with age, and how this affects our ability to combat SARS-CoV-2 infection. This could be crucial in developing effective anti-viral treatments tailored to different age groups, especially for the elderly who are at higher risk of severe COVID-19.”
Co-Senior author, Dr Kerstin Meyer (Wellcome Sanger Institute), said: “By carrying out SARS-CoV-2 infections of epithelial cells in vitro and studying the responses with single cell sequencing, we get a much more detailed understanding of the viral infection kinetics and see big differences in the innate immune response between cell types.”
Children infected with SARS-CoV-2 rarely progress to respiratory failure, but the risk of mortality in infected people over the age of 85 remains high, despite vaccination and improving treatment options.
The research underscores the importance of considering age as a critical factor in both research and treatment of infectious diseases.
Co-senior author, Dr Marko Nikolic (UCL Division of Medicine), said: “It is fascinating that when we take away immune cells from nasal samples, and are only left with nasal epithelial cells grown in a dish, we are still able to identify age-specific differences in our body’s response to the SARS-CoV-2 between the young and elderly to explain why children are generally protected from severe COVID-19.”
Dr Smith added: “Understanding the cellular differences at the initiation of infection is just the beginning. We now hope to investigate the long-term implications of these cellular changes and test therapeutic interventions using our unique cell culture model. This ‘gold-standard’ system is only possible with the support of our funders and the willingness of participants to provide their samples.”
The team suggest that future research should consider how ageing impacts the body’s response to other viral infections.
Source: University College London






