COVID Infection Linked to Increased Risk of Asthma – Vaccination Offers Protection

People who have had COVID are at increased risk of developing certain inflammatory diseases of the airways, such as asthma, hay fever and chronic sinusitis. However, vaccination against the SARS-CoV-2 virus appears to reduce the risk, according to a comprehensive epidemiological study led by researchers at Karolinska Institutet.
The international research team used an electronic health database in the United States, TriNetX, to investigate the link between COVID and so-called type-2 inflammatory diseases, a group of chronic conditions in which the immune system overreacts to allergens or infections.
The researchers compared 973 794 people who had had COVID with 691 270 people who had been vaccinated against the SARS-CoV-2 virus and 4 388 409 healthy controls with no documented infection or vaccination.
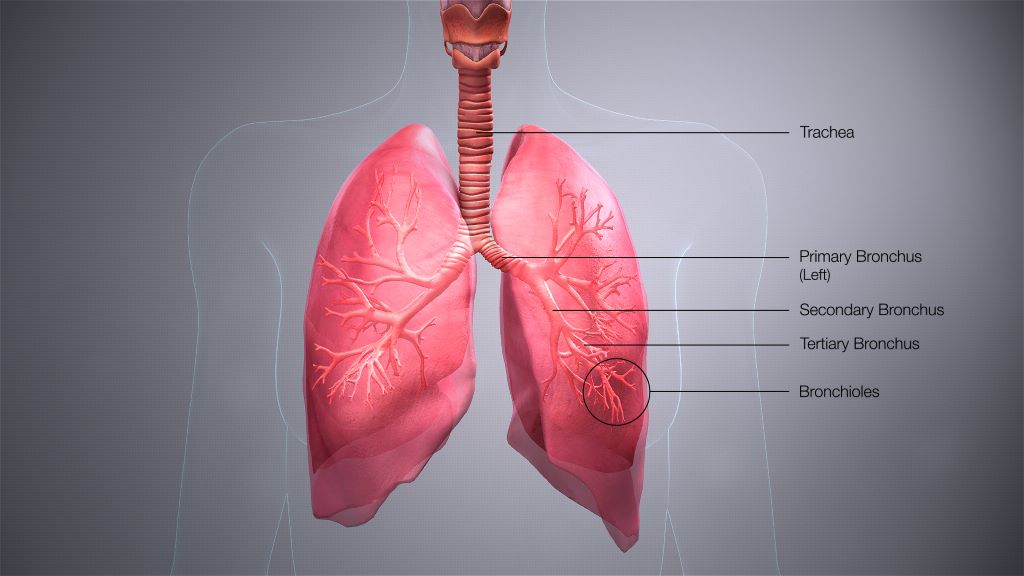
Inflammation in the airways
The results are presented in The Journal of Allergy and Clinical Immunology. People who had had COVID had a 66% higher risk of developing asthma, a 74% higher risk of chronic sinusitis and a 27% higher risk of hay fever compared with healthy controls. However, no increased risk was seen for the skin disease atopic eczema or for eosinophilic oesophagitis, an inflammation of the oesophagus.
“Our results suggest that COVID-19 can trigger type-2 inflammation in the airways, but not in other organs,” says Philip Curman, a physician and researcher at the Department of Medical Epidemiology and Biostatistics at Karolinska Institutet, Sweden, who led the research.
Vaccination against the virus had the opposite effect. The risk of asthma was 32% lower among vaccinated individuals compared with healthy unvaccinated individuals. The risk of sinusitis and hay fever was also slightly lower.
More than twice the risk
When people who had had COVID were compared with vaccinated individuals, an even clearer effect was seen. Infected individuals had more than twice the risk of developing asthma or chronic sinusitis and a 40% higher risk of developing hay fever compared with those who had been vaccinated.
“It is interesting to see that vaccination not only protects against the infection itself, but also appears to provide good protection against certain respiratory complications,” says Philip Curman.
The study is retrospective, i.e. based on data that has already been collected. This means that the researchers cannot draw any firm conclusions about causal links. Another limitation is that some infections may have gone undiagnosed, especially if they were detected through self-testing.
The research was conducted in close collaboration with the University of Lübeck and the Lübeck Institute of Experimental Dermatology in Germany, the Technical University of Madrid in Spain and Bar-Ilan University in Israel. It was mainly funded by the German Research Foundation (Deutsche Forschungsgemeinschaft), Region Stockholm and Karolinska Institutet. Two researchers received travel grants from TriNetX, which provides the database used in the study, and one of the authors is employed by the company.
Source: Karolinska Institutet