New Drug Offers Hope against Untreatable Gonorrhoea

By Catherine Tomlinson for Spotlight
Newly announced results of a pivotal phase 3 trial have demonstrated the effectiveness of a new one-dose treatment for gonorrhoea. The medicine, called zoliflodacin, is the first new drug developed to treat gonorrhoea in over 30 years. More than half of the 930 patients included in the trial were from South Africa, including women, adolescents, and people living with HIV.
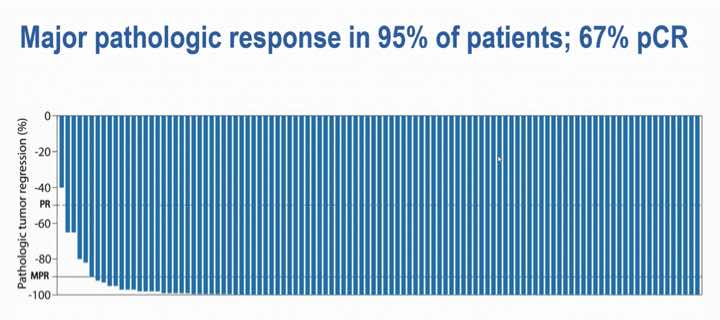
Zoliflodacin, which was shown to be non-inferior to (as good as) the currently used treatment in treating uncomplicated gonorrhoea, provides an important new tool to combat rising rates of drug resistant gonorrhoea. It was found to be generally well tolerated and there were no serious adverse events or deaths recorded in the trial. So far, only top line results have been shared in a media release and the findings have not yet been published in a medical journal. (You can see some technical details of the study design on ClinicalTrials.gov)
The World Health Organization raised the alarm about increasing rates of drug resistant gonorrhoea in 2017, noting the emergence of cases of untreatable gonorrhoea resistant to all available antibiotics. According to the United States Centers for Disease Control and Prevention “medication to treat gonorrhoea has been around for decades, but the bacteria has grown resistant to nearly every drug ever used to treat it”. They say: “only one class of antibiotics known as cephalosporins remains to treat the infection”.
As a drug from a new class of antibiotics, zoliflodacin, offers a new potential treatment for patients whose gonorrhoea was previously untreatable, as well as a new tool for safeguarding the ongoing effectiveness of currently available antibiotics.
How zoliflodacin may change gonorrhoea treatment
Professor Sinead Delany-Moretlwe, Director of Research for Wits RHI and the National Principal Investigator for the trial in South Africa, told Spotlight that while zoliflodacin may be used to treat drug resistant gonorrhoea, it also provides an attractive new treatment option for first-line treatment of gonorrhoea in some countries (in other words, gonorrhoea that is not resistant to other treatments).
Zoliflodacin, which is taken as a single oral dose, is simpler to administer than the current standard of care, which involves a combination of injectable ceftriaxone and oral azithromycin. Removing the need for an injection could simplify the administration of gonorrhoea treatment and improve its uptake.
Using zoliflodacin as first-line gonorrhoea treatment can also help safeguard the ongoing effectiveness of cephalosporins (including ceftriaxone), according to Delany-Moretlwe, which she adds are needed not just for treatment of gonorrhoea, but also other infections.
According to Delany-Moretlwe, because zoliflodacin is the first of a new class of antibiotics with novel mechanisms of action and without existing cross resistance, the hope is that widespread use of zoliflodacin as first-line gonorrhoea treatment will slow the emergence of resistance compared with the medicines currently being used.
The Global Antibiotic Research and Development Partnership (GARDP), a non-profit that sponsored the trial, points out that: “Antimicrobial resistance [AMR] has been around for millions of years, long before the first man-made antibiotics. So, drug-resistant bacteria are inevitable and will eventually affect all antibiotics”. They state: “to beat AMR we need a steady supply of new antibiotics to be developed that are effective against drug-resistant bacteria, particularly for priority pathogens that have the greatest public health impact.”
Gonorrhoea in South Africa
South Africa has incredibly high rates of gonorrhoea, with an estimated 2 million new cases annually. While data on rates of drug resistance in the country is limited, the data that is available indicates that ceftriaxone resistance in the country is low, but azithromycin resistance is concerningly high in some parts of the country.
As there is no routine screening for gonorrhoea in South Africa, linkage to treatment remains a challenge. Currently, diagnosis is largely done through symptomatic reporting by patients. But this approach misses many cases as some patients do not self-report symptoms and some cases of gonorrhoea are asymptomatic.
In 2022, the Southern African HIV Clinicians Society released new guidelines for the management of sexually transmitted infections which called for provider-initiated symptomatic screening and provider-initiated diagnostic screening in high-risk populations.
The country’s new National Strategic Plan on HIV, TB and STIs has set a target to increase the number of pregnant women tested for gonorrhoea from 10% in 2023 to 80% by 2028 and has committed to implementing diagnostic testing in other priority populations, including adolescent girls and young women.
How will new gonorrhoea treatments be commercialised?
Zoliflodacin was developed by GARDP in collaboration with the company Innoviva Specialty Therapeutics. According to GARDP, it holds the rights to register and commercialise zoliflodacin in more than three-quarters of the world’s countries, including all low-income countries, most middle-income countries, and several high-income countries. While, Entasis Therapeutics Limited, an affiliate of Innoviva Specialty Therapeutics, “retains the commercial rights for zoliflodacin in the major markets in North America, Europe, Asia-Pacific, and Latin America”.
South Africa is one of the countries in which GARDP holds the rights to register and commercialise zoliflodacin. It is anticipated that this will be done through selection and licensing of companies to manufacture and supply zoliflodacin in South Africa and other countries where GARDP holds commercialisation rights.
GARDP recently launched a request for proposals from partners that are interested in commercialising zoliflodacin. GARDP has also signed a memorandum of understanding with two generic producers to explore opportunities to commercialise the medicine in low-and-middle-income countries.
While the price that will be offered by commercial partners for the product remains to be seen, it is anticipated that products will be made available at affordable prices in line with GARDP’s goal to ensure that “all GARDP products are available, affordable, and appropriately used across populations that need them”.
“This is the first study to address a World Health Organization priority pathogen that has been sponsored and led by a non-profit organization,” says GARDP.
“This demonstrates that GARDP’s model can play a crucial role in helping to fix the public health failure at the heart of the global AMR crisis,” says Professor Glenda Gray, GARDP board member and President of the South African Medical Research Council.
SA involvement
According to GARDP, South Africa had the highest number of participants in the global trial, across six sites in four provinces: Wits RHI in Hillbrow, Johannesburg; the Desmond Tutu HIV Foundation in Masiphumelele, Cape Town; Setshaba Research Centre in Soshanguve, Gauteng; the SAMRC’s clinical research sites in Botha’s Hill and Tongaat in KwaZulu-Natal; and Ndlovu Research Centre in Groblersdal, Limpopo.
“We have also been able to leverage our HIV experience to build capacity for trials of novel STI technologies, a previously neglected area. Undertaking this vital work on a new treatment for gonorrhoea has also given us the opportunity to focus sharply on the local situation in South Africa,” says Delany-Moretlwe.
Republished from Spotlight under a Creative Commons Licence.
Source: Spotlight