Daytime-only Meals Could Protect People from the Heart Risks of Shift Work

A new study from Mass General Brigham suggests that eating only during the daytime could help people avoid the health risks associated with shift work. Results are published in Nature Communications.
“Our prior research has shown that circadian misalignment – the mistiming of our behavioral cycle relative to our internal body clock – increases cardiovascular risk factors,” said senior author Frank A.J.L. Scheer, PhD, a professor of Medicine at Brigham and Women’s Hospital. “We wanted to understand what can be done to lower this risk, and our new research suggests food timing could be that target.”
Animal studies have shown that aligning food timing with the internal body clock could mitigate the health risks of staying awake during the typical rest time, which prompted Scheer and his colleagues to test this concept in humans.
For the study, researchers enlisted 20 healthy young participants to a two-week in-patient study at the Brigham and Women’s Center for Clinical Investigation. They had no access to windows, watches, or electronics that would clue their body clocks into the time. The effect of circadian misalignment could be determined by comparing how their body functions changed from before to after simulated night work.
Study participants followed a “constant routine protocol,” a controlled laboratory setup that can tease apart the effects of circadian rhythms from those of the environment and behaviours (eg, sleep/wake, light/dark patterns). During this protocol, participants stayed awake for 32 hours in a dimly lit environment, maintaining constant body posture and eating identical snacks every hour. After that, they participated in simulated night work and were assigned to either eating during the nighttime (as most night workers do) or only during the daytime. Finally, participants followed another constant routine protocol to test the aftereffects of the simulated night work. Importantly, both groups had an identical schedule of naps, and, thus, any differences between the groups were not due to differences in sleep schedule.
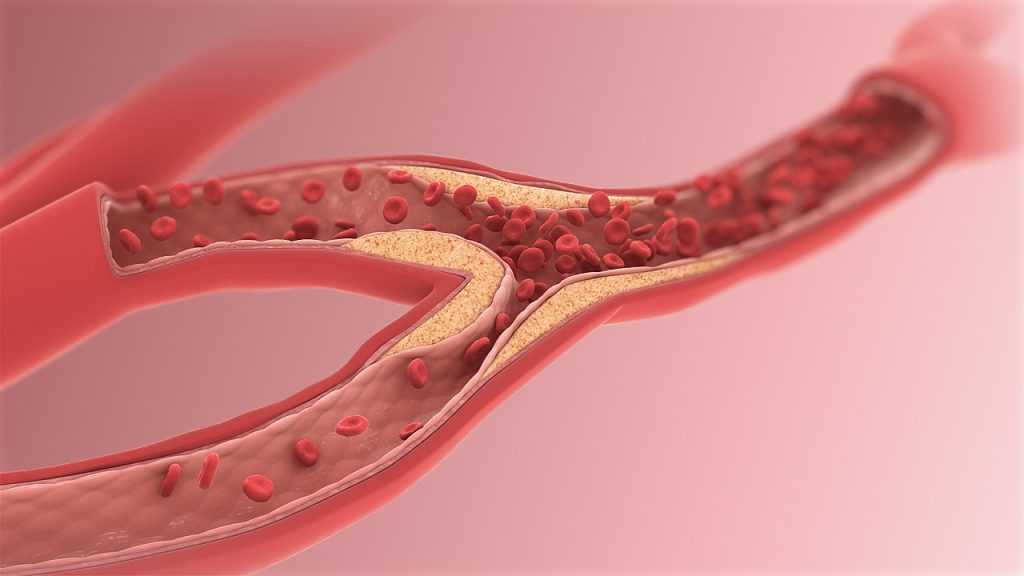
The investigators examined the aftereffects of the food timing on participants’ cardiovascular risk factors and how these changed after the simulated night work. Researchers measured various cardiovascular risk factors, including autonomic nervous system markers, plasminogen activator inhibitor-1 (which increases the risk of blood clots), and blood pressure.
Remarkably, these cardiovascular risk factors increased after simulated night work compared to the baseline in the participants who were scheduled to eat during the day and night. However, the risk factors stayed the same in the study participants who only ate during the daytime, even though how much and what they ate was not different between the groups—only when they ate.
Limitations of the study include that the sample size was small, although of a typical size for such highly controlled and intensive randomised controlled trials. Moreover, because the study lasted two weeks, it may not reflect the chronic risks of nighttime versus daytime eating.
A strength is that the study participants’ sleep, eating, light exposure, body posture, and activity schedule were so tightly controlled.
“Our study controlled for every factor that you could imagine that could affect the results, so we can say that it’s the food timing effect that is driving these changes in the cardiovascular risk factors,” said Sarah Chellappa, MD, MPH, PhD, an associate professor at the University of Southampton, and lead author for the paper.
While further research is necessary to show the long-term health effects of daytime versus nighttime eating, Scheer and Chellappa said the results are “promising” and suggest that people could improve their health by adjusting food timing. They add that avoiding or limiting eating during nighttime hours may benefit night workers, those who experience insomnia or sleep-wake disorders, individuals with variable sleep/wake cycles, and people who travel frequently across time zones.
Source: Mass General Brigham