Talking about HPV, Cervical Cancer and the HPV Vaccine

As the Department of Health gears up for the first round of Human Papilloma Virus (HPV) vaccinations for girls between 9 and 14 from February 3 to March 28, we put the spotlight on HPV and cervical cancer. The focus is on: Empowering, Preventing and Early Detection of cervical cancer. It’s important because cervical cancer kills more South African adolescents and women aged 15 to 44 than any other cancer. It can be successfully treated, if caught early enough but it’s far better to prevent it in the first place.
Dr Themba Hadebe, Clinical and Managed Care Executive at Bonitas, provides some insights and important information about cervical cancer – caused by persistent infection with HPV – why it is essential to screen for the virus and the vaccination that can help prevent it.
Why a vaccine against HPV?
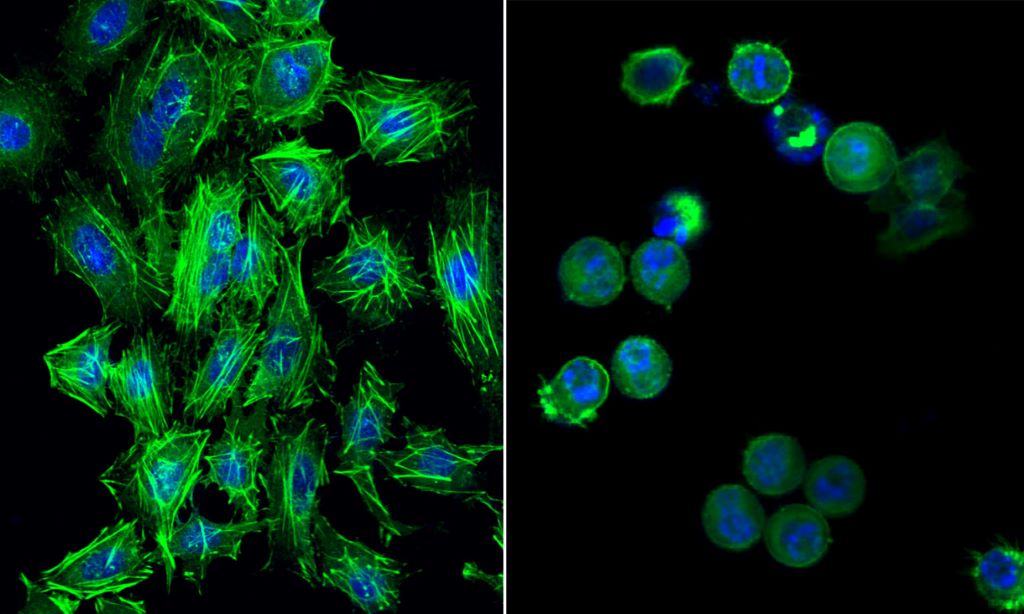
HPV infects the cells of the cervix and, in some cases, the virus can persist – leading to abnormal changes in the cells that may eventually become cancerous. Over 99% of all cervical cancers are caused by persistent infection of high-risk types of HPV, including HPV-16 and HPV-18.
‘To help prevent cervical cancer, we have expanded our preventative care benefits to include the HPV vaccine across all plans,’ says Dr Hadebe. ‘As recommended by The World Health Organization (WHO), this is 2 doses for females aged 9 to 14 years and 3 doses for females aged 15 to 26 years, per lifetime’.
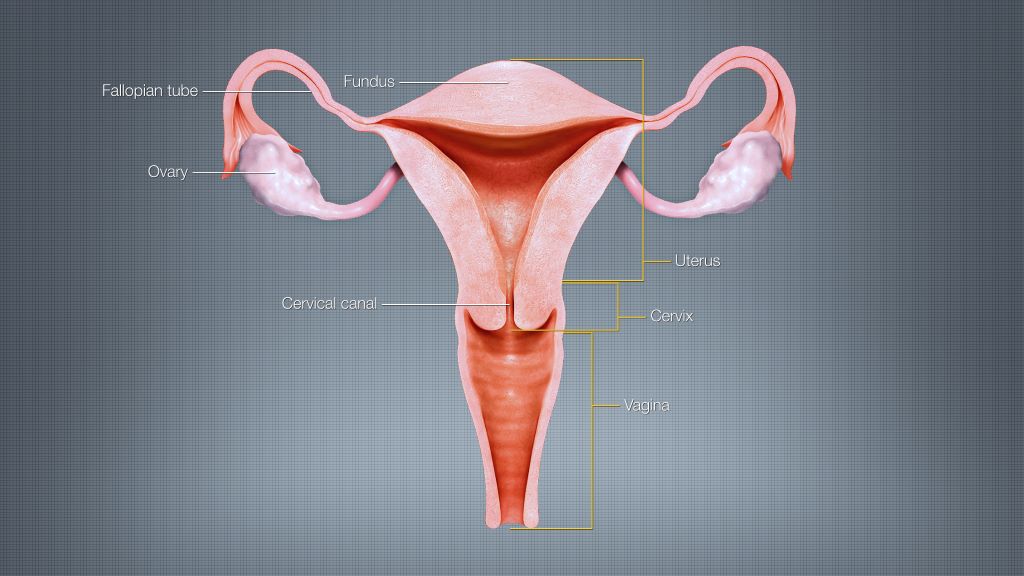
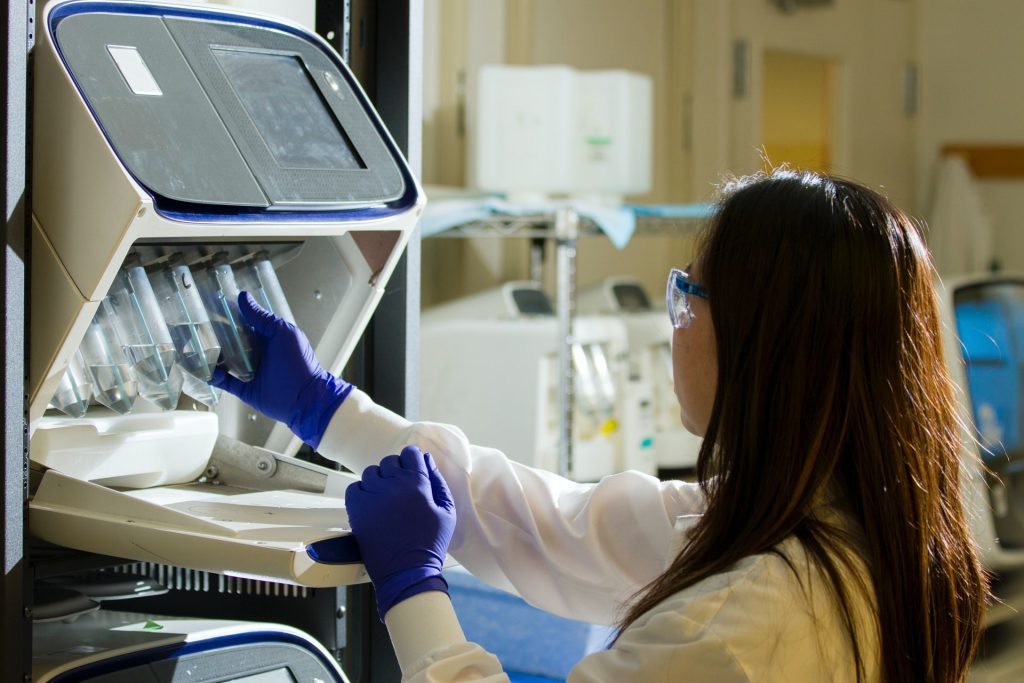
Screening for HPV and cervical cancer: Screening is essential to mitigate the risk of developing cervical cancer and aims to identify cervical cell changes and detect early cervical cancers before they cause symptoms. Two screening tests help with detection:
- Pap smear: Cervical cancer is usually a slow-growing cancer, which may not have immediate symptoms but can be found with regular pap smear tests (a procedure in which cells are scraped from the cervix and looked at under a microscope). The test looks for cell changes (pre-cancers) in the cervix that may progress to cancer if not treated.
- HPV test: This test looks for the virus, particularly HPV-16 and HPV-18 that cause 90% of cervical cancers.
It is recommended that between the ages of 21 and 65, women should have a pap smear every two years and, from the age of 30 onwards, a pap smear and HPV test should be done every 5 years.
Signs and symptoms: The symptoms of the HPV virus can include: Lesions on the genital area as well as darker lesions on other parts of the body, to painful bumps on your upper limbs and skin growths on the balls of the feet and heels.
The power of prevention: ‘Talk to your daughter about important lifestyle choices she must make’, says Dr Hadebe. ‘These may be uncomfortable conversations to have but they’re vitally important to protect her from HPV and subsequent diseases.’ Discussion points include the fact that the HPV vaccination is her best opportunity for protection from the virus. In addition, she needs to consider the following:
- Delay having intercourse until she’s 18: The earlier she starts, the higher her risk of HPV infection
- Use protection every time she is physically intimate: HPV is spread through skin-to-skin contact
- Limit her number of intimate partners
- Avoid smoking: Smoking damages the cells throughout the body, not just those in the lungs. Smoking not only increases her risk for cancer but it also increases her risk of dying from cancer, as well as from other diseases.
- Maintain a healthy weight: The greater your body fat percentage, the higher the risk of cancer. Eating a nutritious, balanced diet and exercising regularly will help her manage her weight and strengthen her immune system.
If you develop cervical cancer: Just like other cancers, cervical cancer is graded according to severity. From in situ, which means it hasn’t spread to nearby tissue, through stage one (it’s still in the original organ and small).
If it progresses, it spreads to the surrounding lymph nodes and, in the most severe form, the cancer has metastasised to surrounding tissues and other lymph nodes.
As cervical cancer develops, the following may occur:
- Abnormal bleeding, for example bleeding after sex
- Pelvic pain unrelated to the menstrual cycle
- Heavy or unusual discharge
- Increased urinary frequency
- Pain during urination
‘Cervical cancer is the most prevalent cancer among women after breast cancer,’ says Dr Hadebe. ‘Yet it has a good chance of being cured, if diagnosed at an early stage and treated promptly. Which is why, it’s important to have regular pap smears to detect any changes in the cervix and to vaccinate young girls to protect them against possible HPV infection.’
Additional information on cervical cancer and HPV can be found on the Bonitas website: www.bonitas.co.za or the Department of Health https://www.health.gov.za