Thoracic Aorta Diameter Can Predict Cardiovascular Risk

A new study in the journal Radiology has found that the diameter of the thoracic aorta can be a biomarker for heart attacks and other adverse cardiovascular events in women and men, and has the advantage of being simple to add on to existing screening.
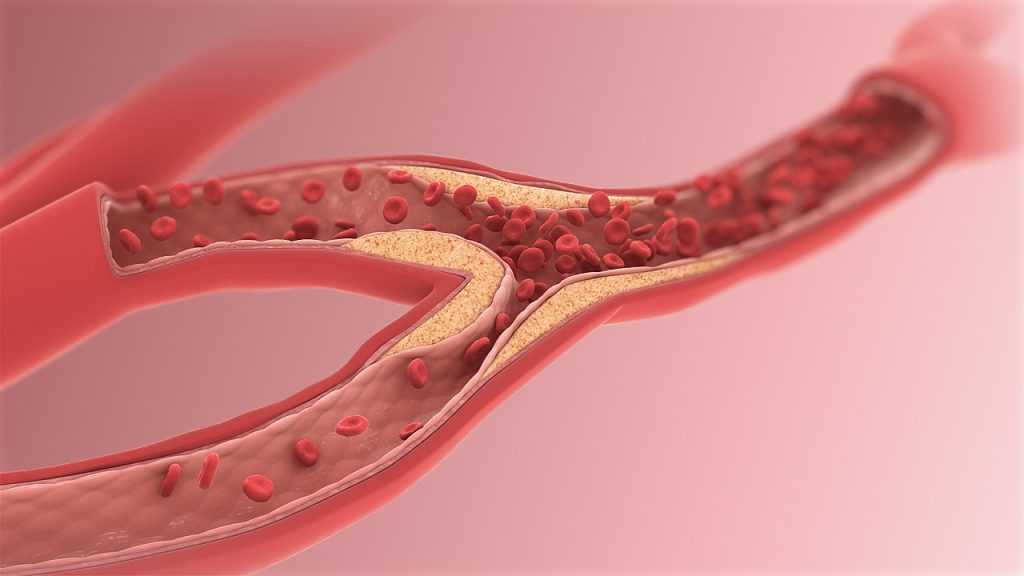
The thoracic aorta is divided into an ascending aorta that rises from the left ventricle of the heart and a descending aorta in the back of the chest.
While the thoracic aorta grows with age, but changes of vessel size and structure, a phenomenon known as vascular remodelling, have a systemic nature involving haemodynamic and biological processes that are also linked to cardiovascular disease.
“While enlargement of the thoracic aorta is a frequent finding in clinical practice, few longitudinal data regarding its long-term prognosis for major cardiovascular disease outcomes at the population level exist,” said study senior author Maryam Kavousi MD, PhD, from University Medical Center Rotterdam.
Dr Kavousi and colleagues assessed these associations in 2178 participants from the population-based Rotterdam Study. Participants underwent multi-detector CT scans between 2003 and 2006 and were followed for an average of 9 years. Thoracic aorta diameters were indexed for body mass index (BMI).
Larger BMI-indexed ascending and descending thoracic aortic diameters were significantly associated with increased risk of adverse cardiovascular outcomes like stroke and death in both women and men.
“Our results suggest that imaging-based assessment of diameter of thoracic aorta can be considered as a risk marker for future cardiovascular disease,” Dr Kavousi said.
In women, greater ascending aortic diameter was associated with 33% higher cardiovascular mortality risk. There seems to be a sex difference in remodelling of the ageing aorta, with faster deterioration in women.
“Ageing could affect aortic health and structure more adversely in women than in men,” Dr Kavousi said.
The study findings suggest that cardiovascular risk assessment associated with thoracic aortic size among asymptomatic women and men could lead to effective, sex-specific prevention strategies.
“As the aortic diameter is significantly related to body size, use of aortic diameters indexed for body measurements could improve its prognostic value for cardiovascular outcomes,” Dr Kavousi said.
Measurement of thoracic aorta size is an easy addition to current screening, the researchers said. The study made use of cardiac CT scans that are already commonly used to assess coronary calcium. Thoracic aortic diameter could also be measured routinely, for example as part of CT-based lung cancer screening.
The current study was based on a single CT-based assessment of thoracic aorta among a large group of participants from the general population, followed up for nine years for incidence of cardiovascular outcomes and mortality. The researchers have recently repeated the CT-based assessment of thoracic aorta among these participants after a median of 14 years.
“This provides an exciting and unique opportunity to study sex-specific risk profiles and patterns of growth in thoracic aorta in the general population,” Dr Kavousi said.