An Inspiration Led to Understanding Metformin’s Anti-tumour Effect

Researchers in Japan have elucidated how the antidiabetic drug metformin exerts an anti-tumour effect as well.
Certain drugs like metformin have recently been found to have anti-cancer properties. Metformin appears to bolster anti-tumour immunity but the underlying immunological mechanisms were a mystery. With all the permutations and combinations of cancer, a blanket, yet targeted therapy would be ideal.
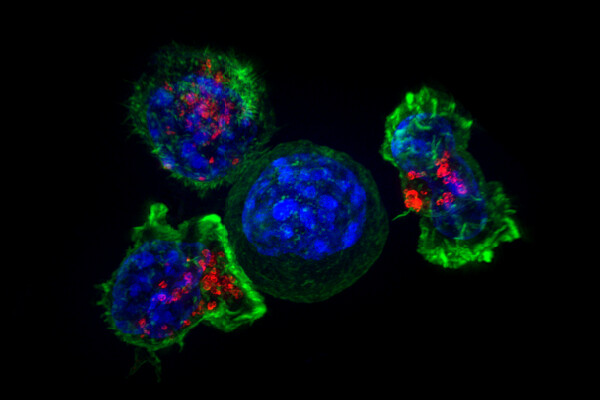
Japanese scientists led by Professor Heiichiro Udono from Okayama University thus decided to address this oncological research question. In their recent study, they looked at how a specific subset of immune cells, called CD8+ infiltrating T-lymphocytes (CD8TIL), which specifically attack tumor cells, behaved in response to metformin. Their findings have been published as a research article in Journal for ImmunoTherapy of Cancer.
Interestingly, Prof. Udono almost gave up on his anti-cancer pursuits, when he lost his own father to cancer. However, a bolt of inspiration came at a conference: “Nearly 10 years ago, a switch turned on in my head when I attended a Keystone Symposia discussing cancer, and hypoxia, held in Banff, Alberta. I realised that we had missed addressing Warburg effect, an effect which bolsters the growth of cancer, in our previous research. So, reverting Warburg effect to normal metabolic profile in cancers became a topic that got me thinking. Surprisingly, I got a hint from the same conference that metformin may aid cancer immunity. So, we got to work!”
Prof Udono and his team got to work, meticulously conducting a series of experiments on cancer cell lines, and ‘knockout gene’ mice, searching for possible biomolecules that result in metformin-dependent anti-tumour immunity. They probed the intracellular mechanisms in CD8TIL, when exposed to metformin, and assessed different biomarkers for growth. Given that CD8TIL produces proteins called interferons to attack cancer cells, they also assessed corresponding levels.
Accordingly, the scientists found that metformin causes the generation of reactive oxygen species in the mitochondria of CD8TIL (mtROS) and increases glycolysis. They also found that mtROS activated growth pathways in CD8TIL, allowing these cells to proliferate. Notably, this is achieved through a transcription factor involved in anti-oxidative stress response, called Nrf. Though metformin did not directly cause apoptosis, ‘cell suicide’ in tumours, it did cause CD8TIL to secrete interferon-ɣ to alter the tumour microenvironment in favour death of tumour cells.
Summing up the findings, Prof. Udono said: “More than anything else, our study provides the knowledge that we can ourselves protect our body from cancer. We hope that this understanding will result in not only the reduction of cancer incidence and improve treatment, but also will help prolong our life.”
The researchers also added that these findings strongly suggest the possibility of using metformin as a drug to strengthen anti-tumour immunity in patients with cancer. The findings appear in the Journal for ImmunoTherapy of Cancer.
Source: EurekAlert!