Passing Through Tight Spaces Make Cancer Cells More Aggressive
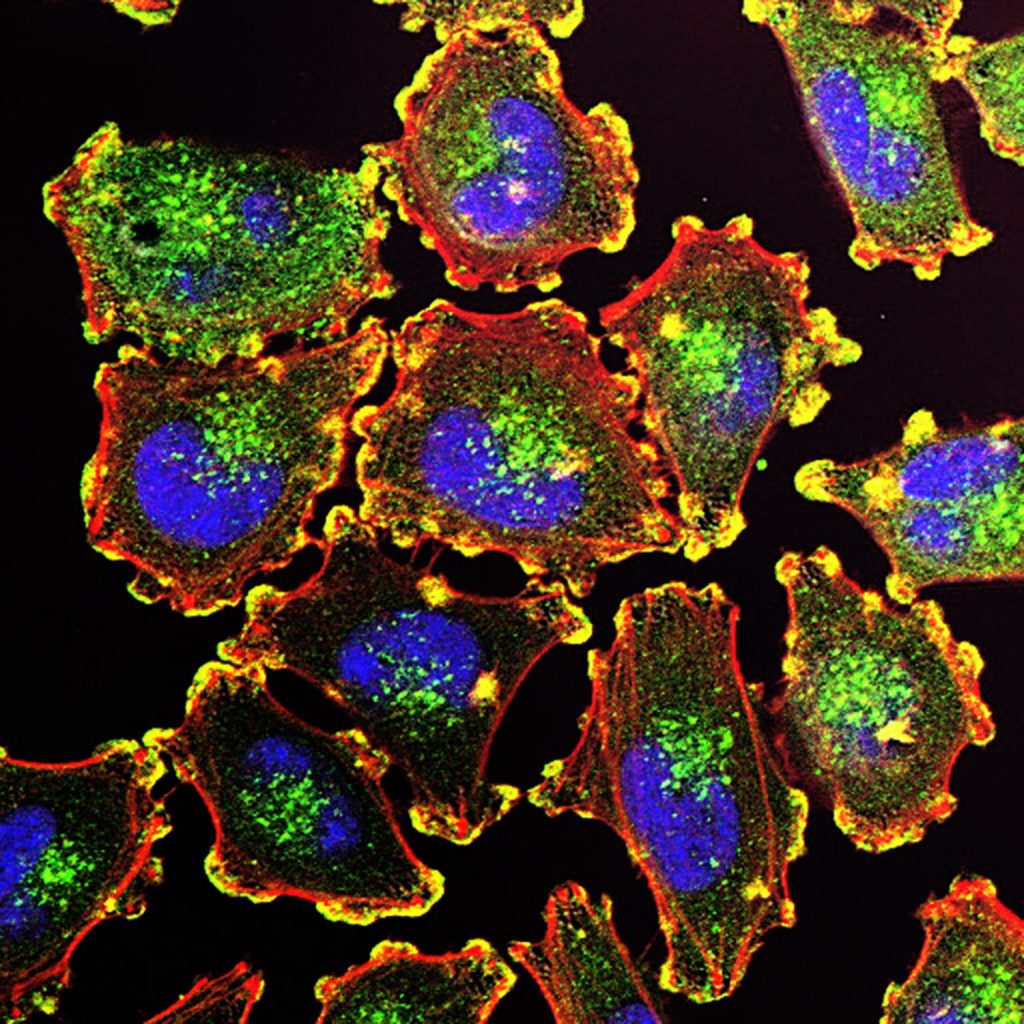
Credit: Bruce Wetzel and Harry Schaefer, National Cancer Institute, National Institutes of Health
Squeezing through tight spaces makes cancer cells more aggressive and helps them evade cell death, a study published in eLife shows.
The researchers’ findings reveal how mechanical stress makes cancer cells more likely to metastasise. While metastasis is the cause of most cancer deaths, there are currently no available cures. However, the new results may help scientists develop novel approaches to treat or prevent metastasis.
When cancer cells escape their tumour or enter called capillaries to spread throughout the body, it can be tight squeeze. The cells have to collapse and change shape – a process called confined migration. The cells must also evade the immune system as they spread outwards.
“Mechanical stress can cause cancer cell mutations, as well as an uncontrolled increase in cell numbers and greater tissue invasion,” explained first author Deborah Fanfone, Postdoctoral Fellow at the Cancer Research Center of Lyon. “We wanted to know if the mechanical stress of confined migration makes cancer cells more likely to metastasise, and how this happens.”
To find out, the researchers forced human breast cancer cells through a membrane with 3µm-sized holes to simulate a confined migration environment. After passing through the membrane just once, the cells became more mobile and resistant to anoikis –a form of programmed cell death that occurs when cells become detached from the extracellular matrix. The cells were also able to escape destruction by immune natural killer cells.
More testing showed that expression of inhibitory-of-apoptosis proteins (IAPs) increased the resistance of cancer cells to anoikis. A new type of cancer drug which degrades IAPs (called a SMAC mimetic), removed this protection in the cancer cells.
The team then examined how these squeezed cells behave when administered to immune-suppressed mice. They found these mice developed more lung metastases than mice that were administered with breast cancer cells that had not been exposed to confined migration.
“By mimicking confined migration, we’ve been able to explore its multifaceted effects on cancer aggressiveness,” says senior author Gabriel Ichim, who leads the Cancer Cell Death team at the Cancer Research Center of Lyon. “We’ve shown how the process boosts survival in cancer cells and makes them more prone to forming deadly metastases.”
The authors add that these results may lead to additional studies of potential metastasis treatments, such as therapies that soften tumours to reduce mechanical stress on cancer cells, or that block IAPs. These include SMAC mimetics, which are currently being tested in clinical trials as a possible new treatment approach.
Source: eLife Sciences