New Trial Flips the Script for Hormonal Treatment of Breast Cancer

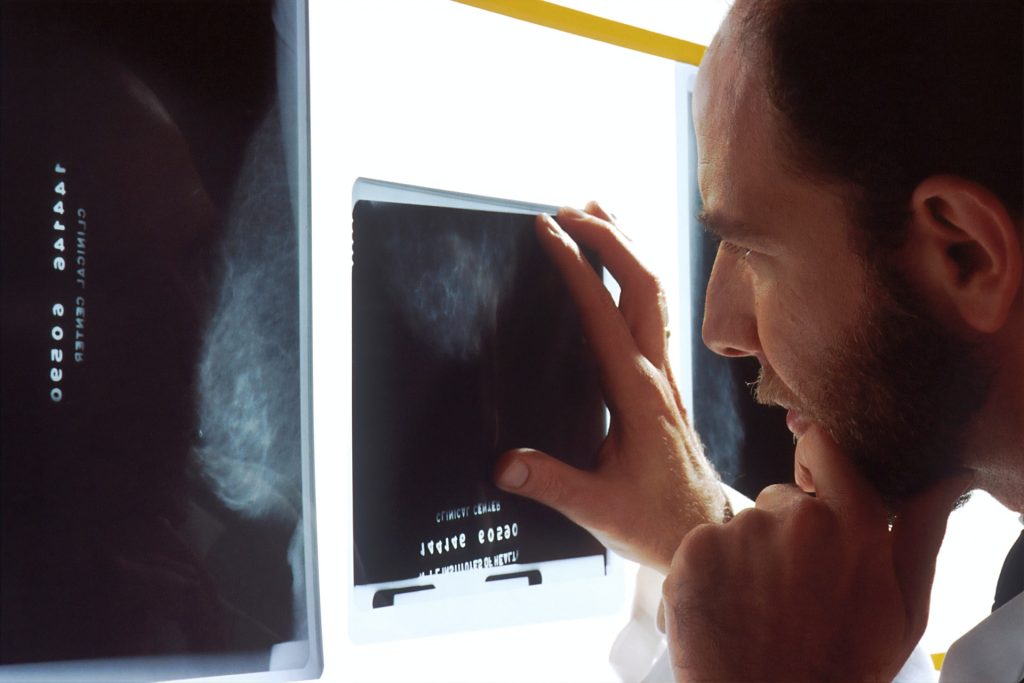
For decades, hormonal treatment of breast cancer has been going in one direction: blocking oestrogen. Now, a global study has discovered there may be another, less toxic way to defeat the most common form of breast cancer. The results, published in The Lancet Oncology, showed that the androgen receptor (AR) agonist enobosarm, is effective against oestrogen receptor-positive (ER+) breast cancer, which constitutes up to 80% of all breast cancer cases.
“The effectiveness of enobosarm lies in its ability to activate the AR and trigger a natural defence mechanism in breast tissue, thereby slowing the growth of ER+ breast cancer, which relies on the hormone oestrogen to grow and spread,” said senior co-author Professor Wayne Tilley, Director of the Dame Roma Mitchell Cancer Research Laboratories at the University of Adelaide.
“This clinical study is supported by our pre-clinical research, previously published in Nature Medicine, which established that the AR is a tumour suppressor in both normal breast tissue and ER+ breast cancer.”
Along with investigators from the University of Adelaide and Dana-Farber Cancer Institute (DFCI) in Boston, USA, the international study also included researchers from the University of Liverpool in the UK and other experts around the world.
The team assessed enobosarm’s efficacy and safety in 136 postmenopausal women with advanced or metastatic ER-positive, HER2-negative breast cancer.
Enobosarm showed significant anti-tumour activity and was well-tolerated by patients, without adversely affecting their quality of life or causing masculinising symptoms.
This discovery represents the first advancement in hormonal treatment of ER+ breast cancer in decades and offers a promising new oral treatment strategy for the most prevalent form of breast cancer.
The new hormonal strategy differs from the existing standard-of-care hormonal treatments, which have been around for decades and involve suppressing oestrogen activity in the body or inhibiting the ER.
Although successful initially, treatments targeting ER can cause severe side effects and treatment-resistant progression of the disease is common.
“Our findings are very promising. They demonstrate that stimulating the androgen receptor pathway with enobosarm can be beneficial,” said senior co-author and study Principal Investigator Dr Beth Overmoyer from DFCI.
“This is the first time a non-oestrogen receptor hormonal treatment approach has been shown to be clinically advantageous in ER+ breast cancer. The study supports further investigation of enobosarm in earlier stages of breast cancer as well as in combination with targeted therapies, such as ribociclib, a CDK 4/6 inhibitor.”
estrogen to grow and spread,” said senior co-author Professor Wayne Tilley, Director of the Dame Roma Mitchell Cancer Research Laboratories at the University of Adelaide.
“The data strongly encourages more clinical trials for AR-stimulating drugs in treating AR-positive and ER-positive breast cancer. The fact that this drug is well-tolerated also opens possibilities for its use in breast cancer prevention,” said co-author Dr Stephen Birrell, a clinical affiliate of the University of Adelaide.
Source: University of Adelaide