Eight or More Drinks per Week Linked to Signs of Injury in the Brain

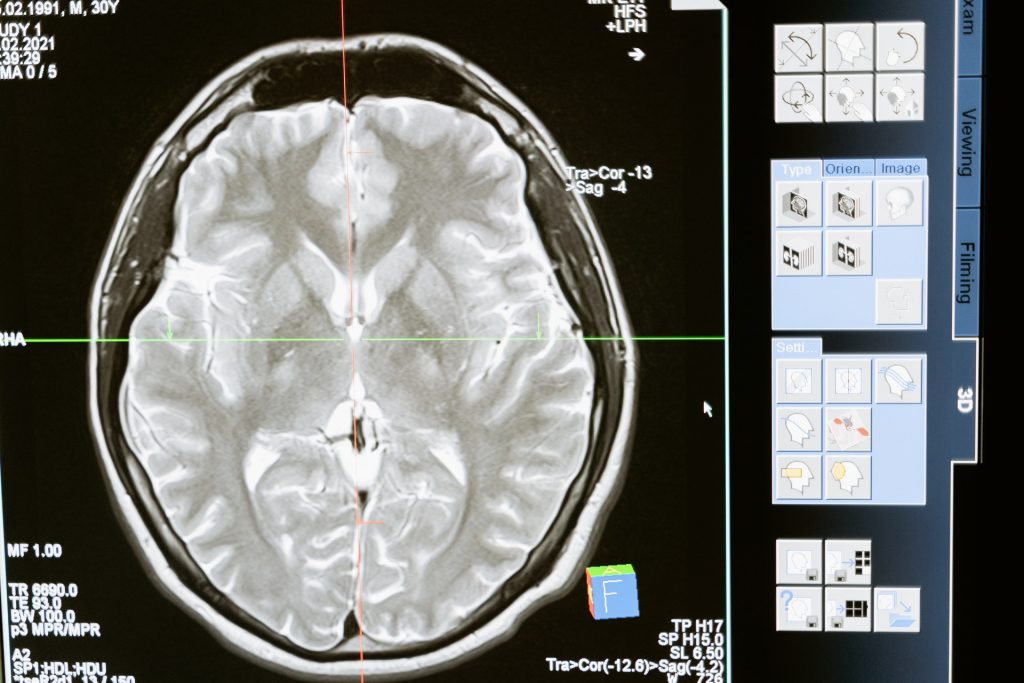
Heavy drinkers who have eight or more alcoholic drinks per week have an increased risk of brain lesions called hyaline arteriolosclerosis, signs of brain injury that are associated with memory and thinking problems, according to a study published on April 9, 2025, online in Neurology®, the medical journal of the American Academy of Neurology (AAN).
Hyaline arteriolosclerosis is a condition that causes the small blood vessels to narrow, becoming thick and stiff. This makes it harder for blood to flow, which can damage the brain over time. It appears as lesions, areas of damaged tissue in the brain.
“Heavy alcohol consumption is a major global health concern linked to increased health problems and death,” said study author Alberto Fernando Oliveira Justo, PhD, of University of Sao Paulo Medical School in Brazil. “We looked at how alcohol affects the brain as people get older. Our research shows that heavy alcohol consumption is damaging to the brain, which can lead to memory and thinking problems.”
The study included 1781 people who had an average age of 75 at death. All had brain autopsies. Researchers examined brain tissue to look for signs of brain injury including tau tangles and hyaline arteriolosclerosis. They also measured brain weight and the height of each participant. Family members answered questions about participants’ alcohol consumption. Researchers then divided the participants into four groups: 965 people who never drank, 319 moderate drinkers who had seven or fewer drinks per week; 129 heavy drinkers who had eight or more drinks per week; and 368 former heavy drinkers.
Researchers defined one drink as having 14 grams of alcohol, which is about 350mL of beer, 150mL of wine or 45mL of distilled spirits. Of those who never drank, 40% had vascular brain lesions. Of the moderate drinkers, 45% had vascular brain lesions. Of the heavy drinkers, 44% had vascular brain lesions. Of the former heavy drinkers, 50% had vascular brain lesions.
After adjusting for factors that could affect brain health such as age at death, smoking and physical activity, heavy drinkers had 133% higher odds of having vascular brain lesions compared to those who never drank, former heavy drinkers had 89% higher odds and moderate drinkers, 60%.
Researchers also found heavy and former heavy drinkers had higher odds of developing tau tangles, a biomarker associated with Alzheimer’s disease, with 41% and 31% higher odds, respectively. Former heavy drinking was associated with a lower brain mass ratio, a smaller proportion of brain mass compared to body mass, and worse cognitive abilities.
No link was found between moderate or heavy drinking and brain mass ratio or cognitive abilities. Justo noted that, in addition to brain injuries, impaired cognitive abilities were observed only in former drinkers. Researchers also found that heavy drinkers died an average of 13 years earlier than those who never drank.
“We found heavy drinking is directly linked to signs of injury in the brain, and this can cause long-term effects on brain health, which may impact memory and thinking abilities,” said Justo. “Understanding these effects is crucial for public health awareness and continuing to implement preventive measures to reduce heavy drinking.”
A limitation of the study was that it did not look at participants before death and did not have information on the duration of alcohol consumption and cognitive abilities.
Source: American Academy of Neurology