Inflammation Pathways are Linked to Changes in Bone Mineral Density over Time
In one of the first studies of its kind, a team of researchers from Keck School of Medicine of USC has found that proteins and pathways involved in inflammation are associated with changes in bone mineral density (BMD) over time. Findings from the study were published in the Journal of Bone and Mineral Research.
The research, which was supported by the National Institutes of Health, could potentially lead to the identification of biomarkers that would serve as early indicators of a person’s risk for bone health issues later in life.
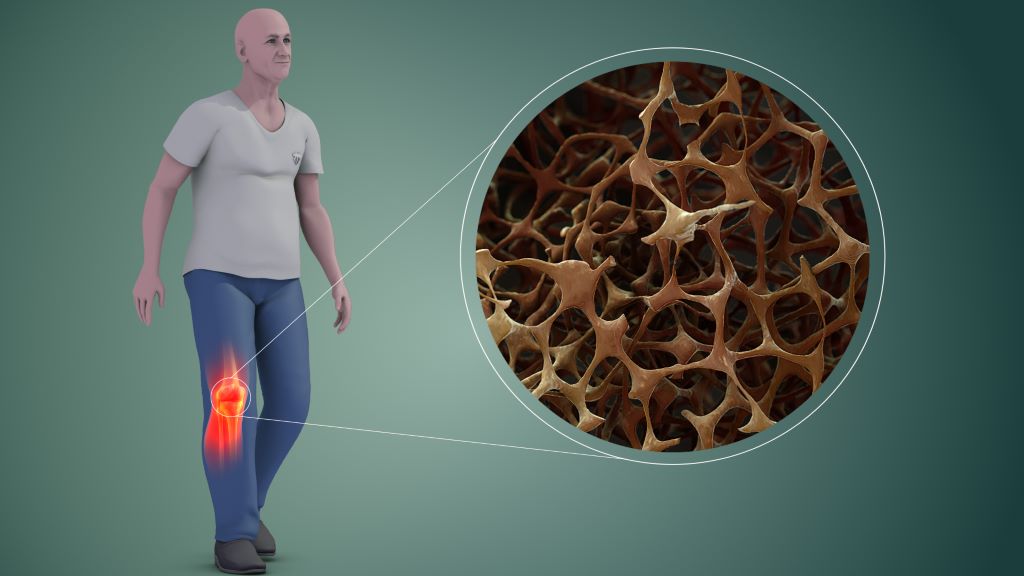
Bone mineral density is a measure of bone strength quantified by the amount of minerals in bone tissue. It peaks during young adulthood and slowly declines over the rest of the life cycle. BMD serves as an important marker for bone health and is commonly used to predict the risk of osteoporosis and other bone health conditions.
“Proteins are also substantial in the formation and maintenance of bone, and recently more studies have been trying to identify individual proteins associated with bone health,” says Emily Beglarian, the lead author and an epidemiology doctoral candidate in the Department of Population and Public Health Sciences at the Keck School of Medicine.
The study followed 304 obese/overweight Latino adolescents between the ages of 8 to 13 at baseline from the Study of Latino Adolescents at Risk for Type 2 Diabetes over an average period of three years. The researchers examined associations between over 650 proteins and annual measures of BMD, making this one of the first studies to evaluate these associations over years of follow-up. The proteins found to be associated with BMD were then inputted into a protein pathway database.
“The software determined what pathways the proteins were involved in within the human body. Our primary findings were that many of the proteins associated with BMD were involved in inflammatory and immune pathways in adolescent populations. There are other studies that found some of these same pathways were associated in older adult populations,” says Beglarian.
Existing studies suggest chronic inflammation can disrupt normal bone metabolism leading to lower BMD.
Importance of inclusive research
Childhood is a critical period for the development of BMD and this period can predict lifelong bone health.
“Until now, existing studies have centred on very specific populations. Most of them have small sample sizes, include either Chinese or non-Hispanic white populations, and focus on older adults – primarily on women because osteoporosis is four times more common in women than men,” says Beglarian.
“This is one of the first studies to investigate associations between proteins and BMD in younger populations. Investigating bone mineral density in early stages of life is important to determine how to address factors that may prevent people from reaching their potential peak bone density,” says Beglarian.
Advancing the understanding of bone health biomarkers
Additionally, Beglarian examined associations between BMD and a subset of protein markers from the initial proteins, in a separate cohort of young adults. Here she found that several proteins had similar associations with lower BMD. Low BMD is a risk factor for development of adulthood osteopenia and osteoporosis.
The study’s findings could potentially inform the development of biomarkers of bone health to identify people at risk that might benefit from intervention.
“It was interesting to see the way in which our study overlapped and differed with existing studies. Previous research was investigating BMD at the end of life when levels are already much lower,” she says. “Through my research I hope to address factors that decrease BMD earlier in life to help people get to their highest potential peak density, so they are set up over the rest of their lifetime to have a higher BMD.”
Source: Keck School of Medicine of USC





