New Treatment-resistant Blood-clotting Disorder Identified
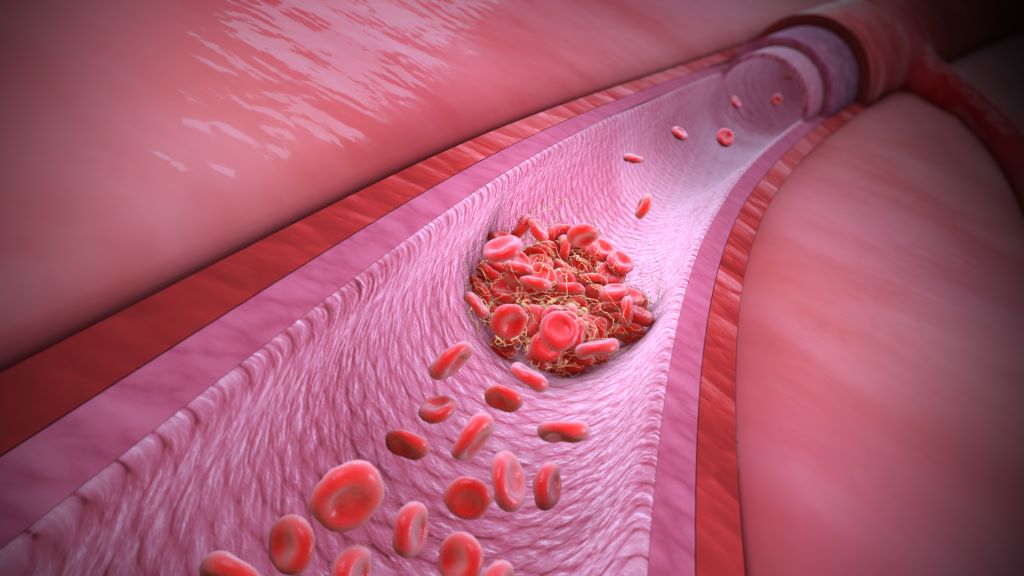
Researchers at McMaster University have made a groundbreaking discovery in the field of haematology, providing an explanation for spontaneous and unusual blood-clotting that continues to occur despite treatment with full-dose blood thinners.
The discovery, published in The New England Journal of Medicine, is expected to influence how doctors test for, and treat patients with, unusual or recurrent blood clotting, with the potential to improve patient outcomes.
Researchers found this new blood clotting disorder to have certain similarities to vaccine-induced immune thrombocytopenia and thrombosis (VITT) – a rare but aggressive clotting disorder that was caused by certain discontinued COVID-19 vaccines.
The research reveals that certain patients can develop severe blood clotting due to antibodies that closely resemble those that cause VITT, even in the absence of known triggers for such antibodies, such as blood thinners (heparin) or prior vaccination.
The newly identified disorder has been termed VITT-like monoclonal gammopathy of thrombotic significance (MGTS).
“Our study highlights the importance of recognising and diagnosing this new blood-clotting disorder,” said Theodore (Ted) Warkentin, co-first author and corresponding author of the study and professor emeritus in the Department of Pathology & Molecular Medicine at McMaster University.
“By understanding how to diagnose VITT-like MGTS, we can develop more effective treatment strategies that go beyond traditional anticoagulation,” said Warkentin, a hematologist in the Department of Medicine based at Hamilton Health Sciences’ Hamilton General Hospital.
Specialized testing was conducted at the McMaster Platelet Immunology Laboratory within the Michael G. DeGroote Centre for Transfusion Research, the only laboratory in Canada with the full repertoire of testing required to characterize the VITT-like antibodies that target the PF4 protein. Researchers performed a detailed analysis of cases exhibiting unusual blood-clotting despite patients being on full-dose blood thinners, focusing on those patients who had unexplained VITT-like antibodies that were detectable for a year or more.
The analyses identified the presence of M (monoclonal) proteins (which typically indicate plasma cell disorders), and together with the persisting VITT-like reactivities over at least 12 months (which is highly unusual for most anti-PF4 antibodies), thus pointing to an ongoing pathological process rather than a short-term anomaly.
The study included a multinational collaboration, with data collected from five patients treated at institutions in Canada, New Zealand, France, Spain, and Germany.
Collaborator Jing Jing Wang of Flinders University in Australia played a crucial role in proving for each patient that the M proteins are the pathological VITT-like antibodies. Collaborator Andreas Greinacher of Greifswald University in Germany helped in identifying similar cases in his anti-PF4 reference lab.
“The findings of this study underscore our ability to leverage fundamental molecular and biochemical science to unravel disease mechanisms,” said Ishac Nazy, co-lead author of the study and scientific director of the McMaster Platelet Immunology Laboratory and co-director of the Michael G. DeGroote Centre for Transfusion Medicine.
“This approach enables precise patient diagnosis and informs timely treatment strategies, even for previously unidentified diseases, exemplifying true bench-to-bedside translational medicine,” said Nazy, associate professor in the Department of Medicine at McMaster.
A remarkable observation was that each of the patients had failed blood thinning treatment, but they showed some benefit with unusual treatments, such as high-dose intravenous immunoglobulin (IVIG), Bruton tyrosine kinase inhibitors (ibrutinib), and plasma cell–targeted myeloma therapy. The existence of this novel blood clotting disorder has important implications for how health care providers will evaluate patients who develop unusual or difficult to treat blood clots in the future.
Source: McMaster University

