Breaching Stubborn Bacterial Biofilms with a ‘Trojan Horse’
A new study has tricked bacteria into sending death signals to stop the growth of biofilms that lead to deadly infections. The discovery by Washington State University researchers could someday be harnessed as an alternative to antibiotics for treating difficult infections.
Reporting in the journal, Biofilm, the researchers used the messengers, which they named death extracellular vesicles (D-EVs), to reduce growth of the bacterial communities by up to 99.99% in laboratory experiments.
“Adding the death extracellular vesicles to the bacterial environment, we are kind of cheating the bacteria cells,” said Mawra Gamal Saad, first author on the paper and a graduate student in WSU’s Gene and Linda Voiland School of Chemical Engineering and Bioengineering.
“The cells don’t know which type of EVs they are, but they take them up because they are used to taking them from their environment, and with that, the physiological signals inside the cells change from growth to death.”
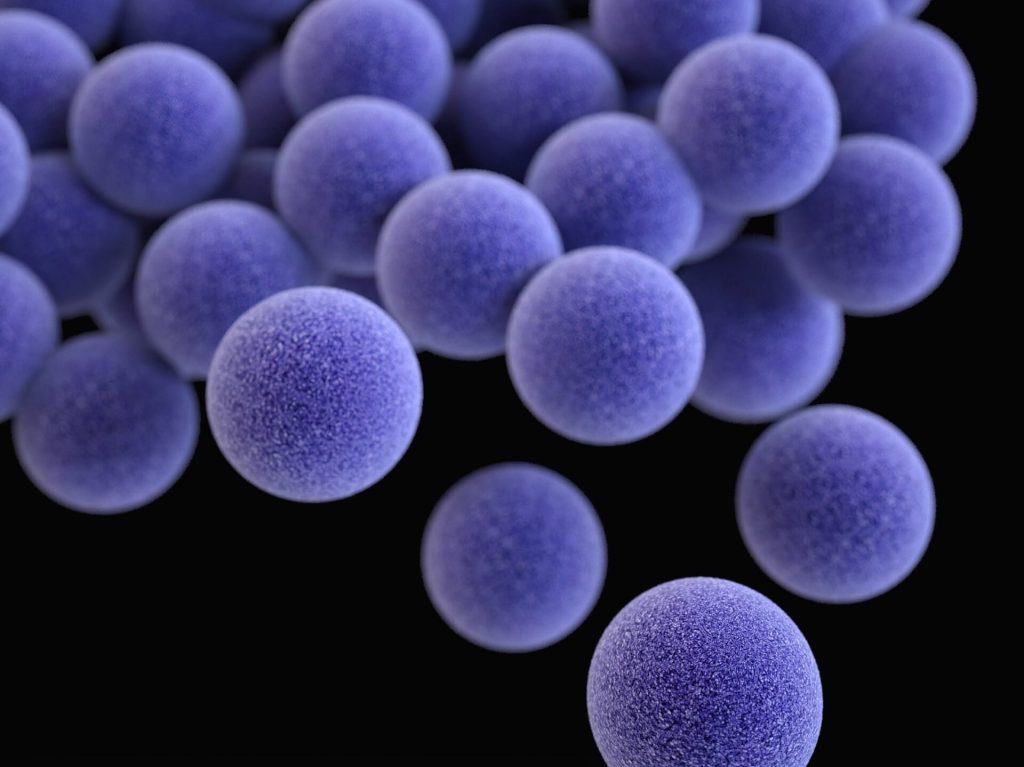
Bacterial resistance is a growing problem around the world. In the US, at least 2 million infections and 23 000 deaths are attributable to antibiotic-resistant bacteria each year, according to the U.S. Centers for Disease Control.
When antibiotics are used to treat a bacterial infection, some of the bacteria can hide within their tough-to-penetrate biofilm. These subpopulations of resistor cells can survive treatment and are able to grow and multiply, resulting in chronic infections.
“They are resistant because they have a very advanced and well-organised adaptive system,” said Saad.
“Once there is a change in the environment, they can adapt their intracellular pathways very quickly and change it to resist the antibiotics.”
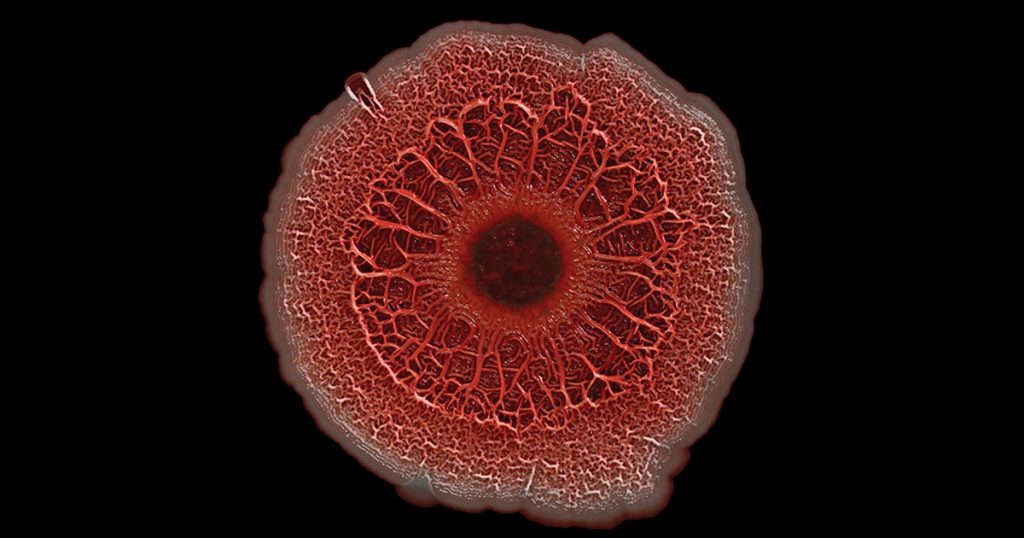
In their new study, the researchers discovered that the extracellular vesicles are key to managing the growth of the protective biofilm.
The vesicles, tiny bubbles from 30 to 50nm or about 2000 times smaller than a strand of hair, shuttle molecules from cells, entering and then re-programming neighbouring cells and acting as a cell-to-cell communications system.
As part of this study, the researchers extracted the vesicles from one type of bacteria that causes pneumonia and other serious infections.
They determined that the bacteria initially secrete vesicles, called growth EVs, with instructions to grow its biofilm, and then later, depending on available nutrients, oxygen availability and other factors, send EVs with new instructions to stop growing the biofilm.
The researchers were able to harness the vesicles with the instructions to stop growth and use them to fool the bacteria to kill off the biofilm at all stages of its growth.
Even when the biofilms were healthy and rapidly growing, they followed the new instructions from the death EVs and died. The death EVs can easily penetrate the biofilm because they are natural products secreted by the bacteria, and they have the same cell wall structure, so the cells don’t recognise them as a foreign enemy.
“By cheating the bacteria with these death EVs, we can control their behaviour without giving them the chance to develop resistance,” said Saad.
“The behavior of the biofilm just changed from growth to death.”
WSU Professor and corresponding author Wen-Ji Dong, who has been studying the vesicles for several years initially thought that all of the bacterial-secreted vesicles would promote cell growth.
The researchers were surprised when they found that older biofilms provided instructions on shutting themselves down.
“So now we’re paying attention to the extracellular vesicles secreted by older biofilms because they have therapeutic potential,” he said.
Source: Washington State University