In Obesity or Not, Individuals Prefer High-calorie Food
Calorie content drives food preference despite similar taste in individuals with and without obesity

Higher calorie foods were preferred among individuals with and without obesity despite similar taste and texture, according to a study published December 17th in the open-access journal PLOS Biology by Albino Oliveira-Maia from the Champalimaud Foundation, Portugal, and colleagues.
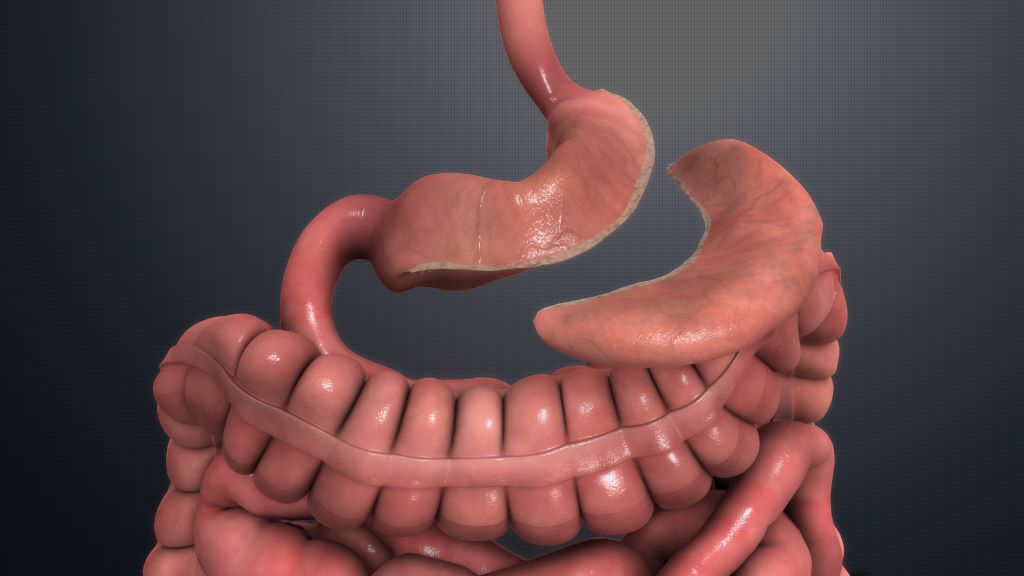
Eating sends signals to the brain with information about a food’s energy content, which can influence food preferences irrespective of flavor. People with obesity often have impairments in areas of the brain where dopamine is released, which may drive reward-related eating and a preference for energy-dense foods rich in fat and sugars. Weight loss due to bariatric surgery has been associated to a normalization of reward-related eating with a shift of preferences toward healthier options, but the underlying mechanisms are not well understood.
In this study, after examining a large group of healthy volunteers, researchers compared food preferences in three groups: 11 individuals with obesity, 23 post-bariatric surgery patients, and 27 non-obese control subjects. They gave participants sweetened low-fat yogurt with and without maltodextrin (a carbohydrate that adds calories to the yogurt with no impact on taste or texture). Participants ate the yogurt at home, alternating between the maltodextrin-containing and -free yogurt. All three groups ate more of the maltodextrin-containing yogurt, despite rating both as equally pleasant. Somewhat unexpectedly, the effects of maltodextrin on yogurt consumption were similar in individuals with obesity relative to their non-obese counterparts.
The study also used radioactive iodine labelling and single photon emission computed tomography to visualise dopamine receptors in the brain. Consistent with previous studies, individuals with obesity had lower dopamine receptor availability than non-obese controls. Dopamine receptor availability was similar in the surgical and non-obese groups and was associated with more restrained eating. These results suggest that obesity-related brain changes can be reversed after bariatric surgery, potentially impacting the amount of food consumed but not necessarily the types of food preferred.
The authors add, “We were very intrigued that, while behaviour was guided towards eating yoghurts with higher energy-content, this did not seem to be a result of explicit choices, since consistent changes in pleasantness of flavours enriched with carbohydrates were not found. Importantly, this behaviour was maintained in patients with obesity and after weight-loss surgery, even though there were important differences in their brain dopaminergic system.”
Provided by PLOS