The Untapped Potential of Phages for the Treatment of Atopic Dermatitis

Researchers in Austria have discovered a new approach to treating atopic dermatitis: bacteriophages, which colonise the skin as viral components of the microbiome and can drive the development of innovative atopic dermatitis therapies. The research results were recently published in the scientific journal Science Advances.
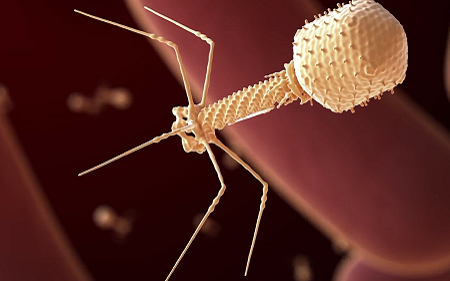
Until now, the importance of bacteriophages in the human body has been known primarily from analyses of the intestine. In the search for innovative therapeutic measures for atopic dermatitis (AD), the MedUni Vienna research team led by Wolfgang Weninger, Head of the Department of Dermatology, has now investigated the interaction of phages and bacteria in the skin for the first time. After all, it has long been known that the progression of AD is accompanied by massive changes in the skin microbiome. The microbiome is the sum of all microorganisms on the skin and has been primarily investigated for its bacterial constituents. It has been unknown whether viruses also contribute to the nature of the bacterial microbiome in healthy and diseased skin. Phages are viruses of different types and functions whose sole aim is to infect bacteria, thereby either destroying them – or stimulating them to multiply.
New phages identified
“In our study, we discovered previously unknown phages in the microbiome of the skin samples of AD patients, which help certain bacteria to grow faster in different ways,” note first authors Karin Pfisterer and Matthias Wielscher from the Department of Dermatology at MedUni Vienna. The resulting shift in the balance between phages and bacteria was not detected in the comparative samples from healthy individuals and may be one explanation for the overpopulation of the skin microbiome with bacteria called Staphylococcus aureus found in AD. These findings contribute significantly to a better understanding of the skin bioflora in AD patients and pave the way for the development of new targeted therapeutic interventions: By identifying and culturing phages specialised for Staphylococcus aureus, a promising new option is available.
Specialists for targeted therapy
Bacteriophages are found not only in the body, but in every habitat populated by bacteria. There are a staggering 1031 different phage species. One of their characteristics is that they prove to be extremely specific when it comes to choosing their target of infection: most phages specialise in a particular genus, and in many cases in only a single species of bacteria. While that makes it a challenge for scientists to identify the type of phage needed for a particular purpose, it also enables them to use them in a targeted manner. Bacterial viruses do not make any difference between antibiotic-resistant and other bacteria, thus they are being researched as possible weapon in the fight against multi-resistant pathogens. Further studies are now planned to confirm phage therapy for topical use in atopic dermatitis.
Source: Medical University of Vienna