Multiple Sclerosis Drug Ocrelizumab Works by Reshaping the Immune System

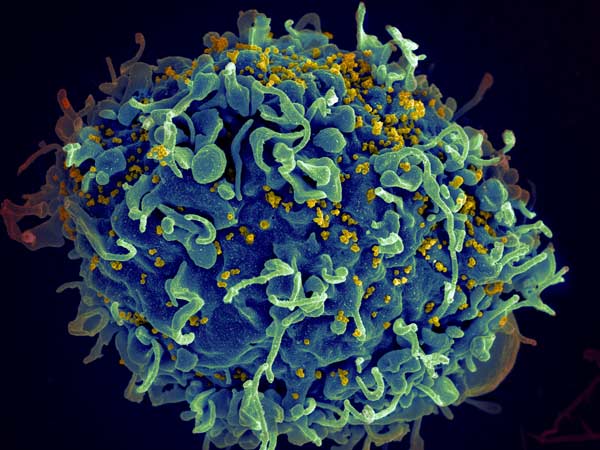
When ocrelizumab became the first FDA-approved treatment for early forms of multiple sclerosis (MS) in 2017, it offered patients immense hope. The long-awaited drug is a monoclonal antibody that depletes B cells – the immune cells that drive MS progression. Exactly how ocrelizumab does this, however, remains unclear.
In a new study published in The Journal of Clinical Investigation, Yale scientists begin to answer this question. By using single-cell RNA sequencing, a technique that provides a window into the gene expression in individual cells, the researchers laid out a detailed view of how ocrelizumab achieves its therapeutic effects.
“The surprise was that the drug doesn’t work at all the way we thought it was working,” says David A. Hafler, MD, Professor of Neurology at Yale School of Medicine, who led the study. “We knew what the end result was and that the drug was enormously effective in patients. But what’s driving the drug’s action is a type of white blood cell in the central nervous system. No one would ever hypothesise that.”
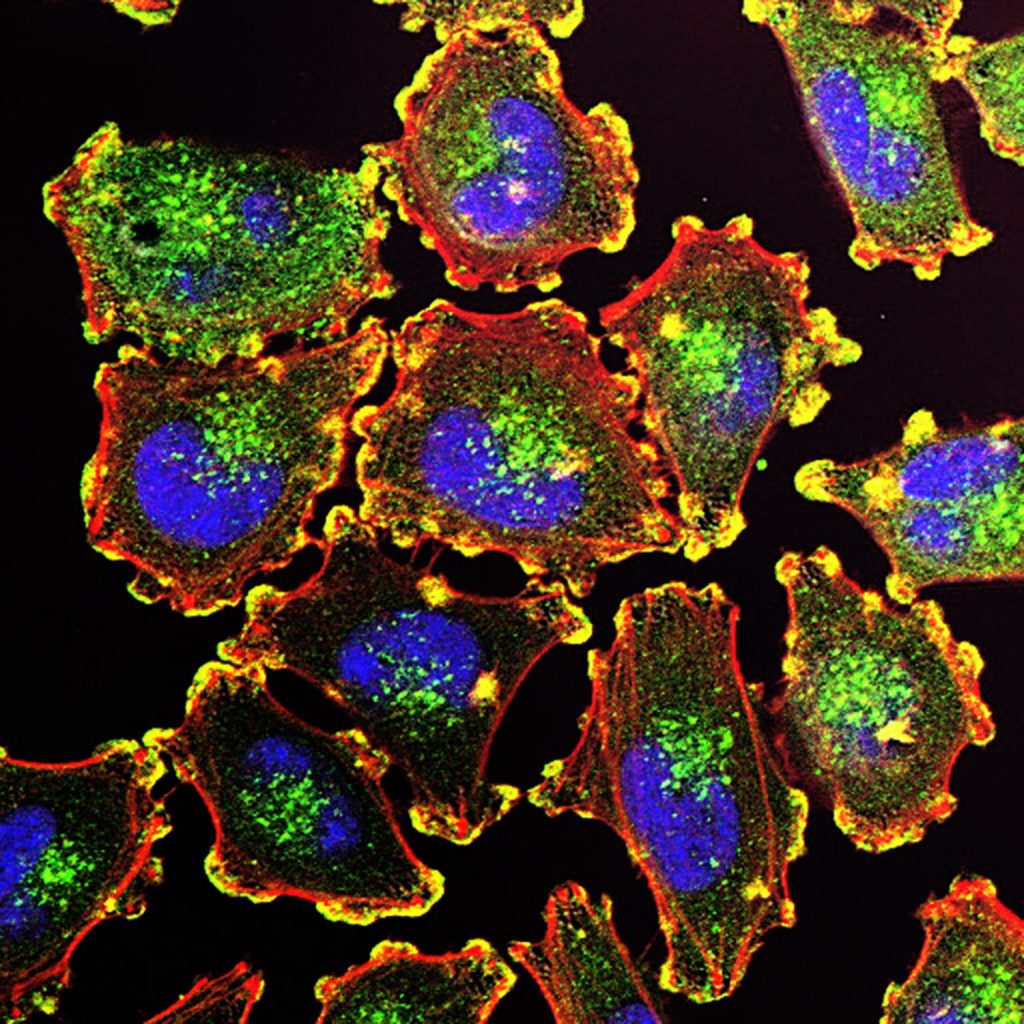
The roles of T cells and B cells in multiple sclerosis
B and T cells have closely intertwined roles in the immune system. B cells are critical cells that recognise foreign objects, bind them, and present them to T cells, which then signal other immune cells to take action. But this relationship goes awry in disease.
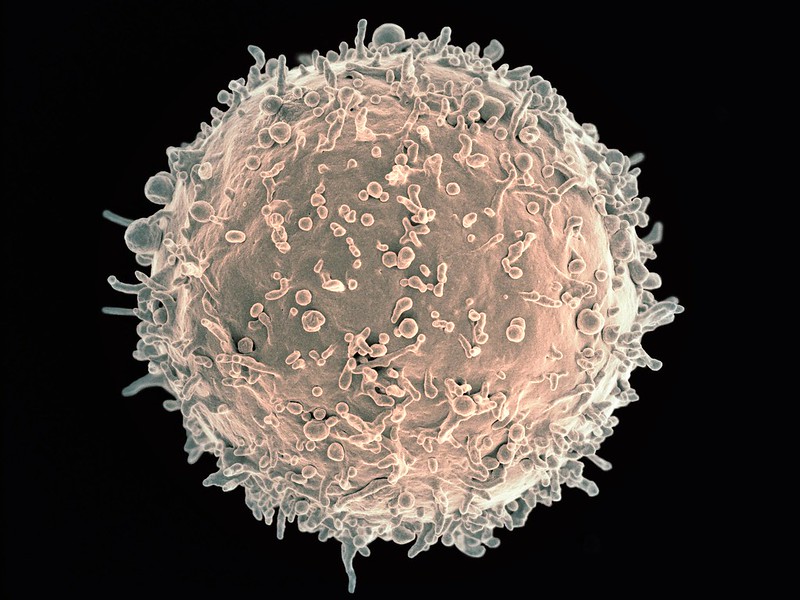
In MS, abnormally active B cells trigger T cells to attack the myelin sheath, the protective layer of nerve fibres, leading to neurological symptoms, such as loss of vision, muscle weakness, and cognitive impairment. More than two decades ago, Hafler and his team discovered this was due to defects in regulatory T cells, which normally put the brake on immune responses, but when defective, unleash immune cells that mistakenly target the body’s own tissues.
In the early stages of MS, both B and T cells are deemed to be the drivers of the disease. Once the disease progresses to a neurodegenerative stage, other inflammatory processes become more prominent.
“Once you enter the neurodegenerative phase of the disease, it is much more difficult to stop the process,” Hafler says. “What we’ve learned is that the earlier you treat the disease, the better the outcome.”
Ocrelizumab binds to the surface of B cells, leading to their destruction. And especially for people in the early stages of MS, it can be quite effective. “The drug works incredibly well,” Hafler says. But Hafler and his team found that ocrelizumab was doing far more than just controlling B cells.
In the new study, the researchers analysed the blood and cerebrospinal fluid of 18 patients, all of whom had an early-onset form of multiple sclerosis in which patients cycle between periods of disease remission and relapse. The scientists measured the cell type-specific changes in protein expression before and after the patients received six months of ocrelizumab, in an effort to identify immune molecules that might change in response to the drug.
They discovered that the reduction in B cells driven by ocrelizumab led to an increase in the pro-inflammatory molecule TNF-α. This was unexpected because TNF-α has been shown to trigger the immune system and exacerbate inflammation in certain diseases. In fact, medications that block the activity of TNF-α are typically used for treating various autoimmune diseases such as rheumatoid arthritis and inflammatory bowel disease.
As they looked further, the researchers found that by inducing TNF-α, ocrelizumab led to an increase in a specific type of regulatory T cell. This, in turn, curbed the circulation of T cells that attack the myelin.
“This unpredicted increase in TNF-α shows that ocrelizumab works in a paradoxical way,” says Hafler.
Understanding the cause of multiple sclerosis
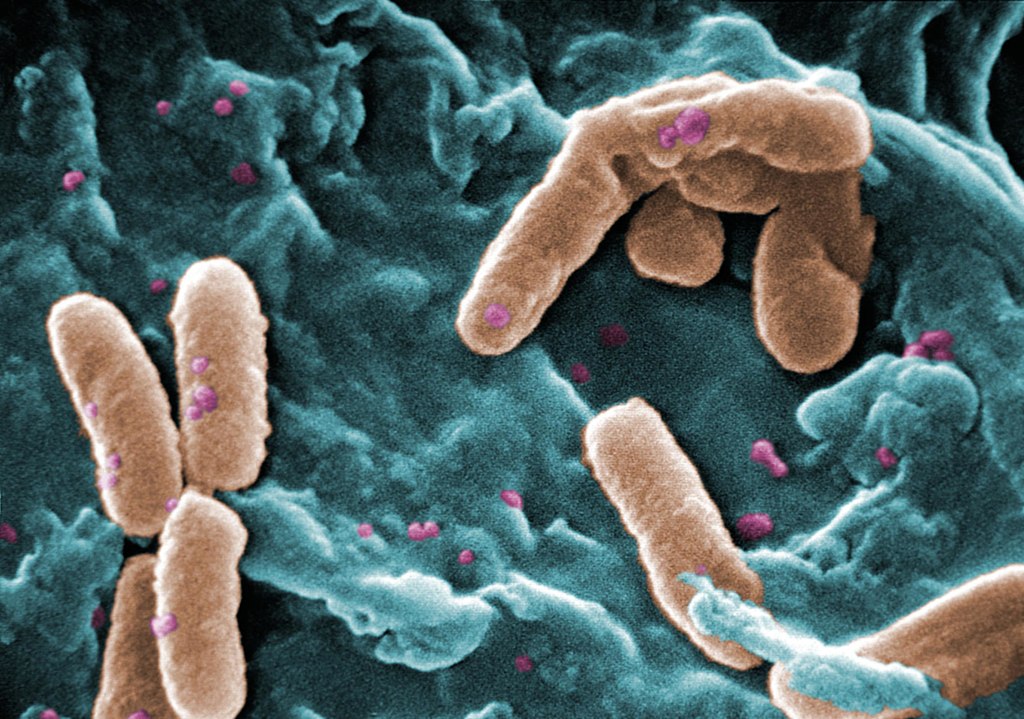
One of the current working models of MS suggests that the disease originates from the Epstein-Barr virus. “How the Epstein-Barr virus triggers the disease is a point that we don’t yet understand,” Hafler says. However, there is a strong body of evidence to show that the virus infects B cells. Therefore, understanding how a B cell-depleting drug affects T cell activity may lead to further explanations.
The current finding also explains why a fifth of the genes linked to MS risk involve the TNF pathway and why many of those genetic changes are protective in other diseases, such as inflammatory bowel diseases.
“This shows that biology has a richness to it,” Hafler says. “When these molecules are made, where they’re made, and what cell they’re working on have very different effects.”
Hafler suspects that ocrelizumab might be acting through other mechanisms as well, an inkling that motivates his lab to continue their investigation. “For something to work that well, there must be other things going on,” he says.
The team is now beginning to study the pathogenesis of MS in a large cohort of women who have at least one parent with the disease. By following the genetic evolution of the disease, the scientists are hoping to better understand how B cells change the immune landscape in real time.
“This study is only one piece of the puzzle,” Hafler says. “We’ll continue to look for other pieces.”
Source: Yale School of Medicine