Study Explains a Link between COVID and Increased Cardiovascular Risk

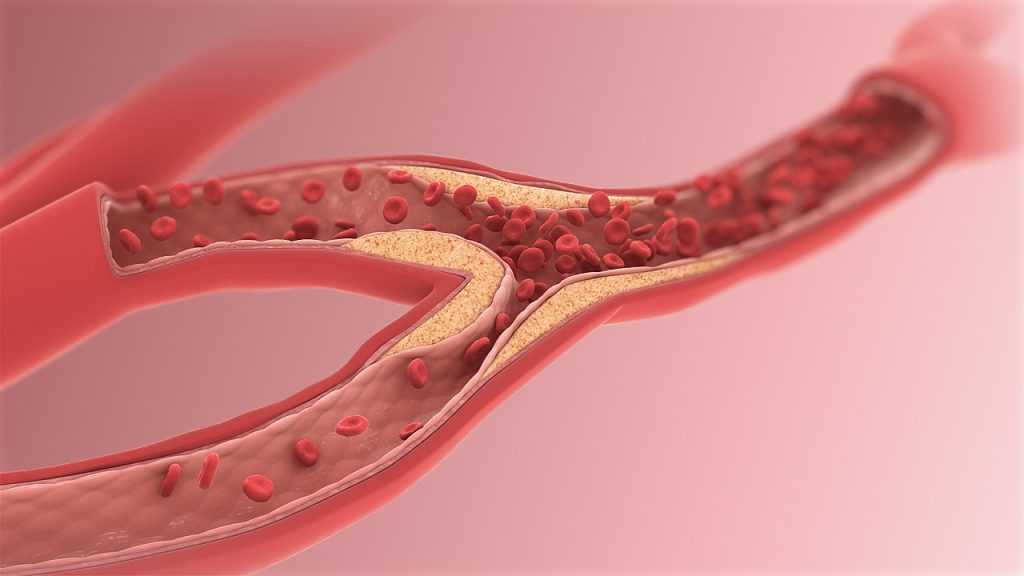
A study published in the journal Nature Cardiovascular Research shows that SARS-CoV-2 can directly infect the arteries of the heart and cause the fatty plaque inside arteries to become highly inflamed, increasing the risk of heart attack and stroke. The findings may help explain why certain people who get COVID have a greater chance of developing cardiovascular disease, or if they already have it, develop more heart-related complications.
In the National Institutes of Health (NIH)-funded study, researchers focused on older people with atherosclerotic plaque, who died from COVID. However, because the researchers found the virus infects and replicates in the arteries no matter the levels of plaque, the findings could have broader implications for anybody who gets COVID.
“Since the early days of the pandemic, we have known that people who had COVID have an increased risk for cardiovascular disease or stroke up to one year after infection,” said Michelle Olive, PhD, acting associate director of the Basic and Early Translational Research Program at the National Heart, Lung, and Blood Institute (NHLBI), part of NIH. “We believe we have uncovered one of the reasons why.”
Though previous studies have shown that SARS-CoV-2 can directly infect tissues such as the brain and lungs, less was known about its effect on the coronary arteries. Researchers knew that after the virus reaches the cells, the body’s immune system sends in macrophages to help clear the virus. In the arteries, macrophages also help remove cholesterol, and when they become overloaded with cholesterol, they morph into a specialised type of cell called foam cells.
The researchers thought that if SARS-CoV-2 could directly infect arterial cells, the macrophages that normally are turned loose might increase inflammation in the existing plaque, explained Chiara Giannarelli, MD, PhD, associate professor in the departments of medicine and pathology at New York University’s Grossman School of Medicine and senior author on the study. To test their theory, Giannarelli and her team took tissue from the coronary arteries and plaque of people who had died from COVID and confirmed the virus was in those tissues. Then they took arterial and plaque cells – including macrophages and foam cells – from healthy patients and infected them with SARS-CoV-2 in a lab dish. They found that the virus had also infected those cells and tissues.
Additionally, the researchers found that when they compared the infection rates of SARS-CoV-2, they showed that the virus infects macrophages at a higher rate than other arterial cells. Cholesterol-laden foam cells were the most susceptible to infection and unable to readily clear the virus. This suggested that foam cells might act as a reservoir of SARS-CoV-2 in the atherosclerotic plaque. Having more build-up of plaque, and thus a greater number of foam cells, could increase the severity or persistence of COVID.
The researchers then looked at the predicted inflammation in the plaque after infecting it with the virus. They observed the release of inflammatory cytokines, also known to promote the formation of even more plaque. The cytokines were released by infected macrophages and foam cells. The researchers said this may help explain why people who have underlying plaque buildup and then get COVID may have cardiovascular complications long after getting the infection.
“This study is incredibly important as it adds to the larger body of work to better understand COVID,” said Olive. “This is just one more study that demonstrates how the virus both infects and causes inflammation in many cells and tissues throughout the body. Ultimately, this is information that will inform future research on both acute and Long COVID.”
Though the findings conclusively show that SARS-CoV-2 can infect and replicate in the macrophages of plaques and arterial cells, they are only relevant to the original strains of SARS-CoV-2 that circulated in New York City between May 2020 and May 2021. The study was conducted in a small cohort of older individuals, all of whom had atherosclerosis and other medical conditions; therefore, the results cannot be generalised to younger, healthy individuals.
Source: National Institutes of Health