Research Reveals New Insights into how LDL Cholesterol Works in the Body
National Institute of Health (NIH) scientists have made a significant breakthrough in understanding how “bad” cholesterol, known as low-density lipoprotein-cholesterol or LDL-C, builds up in the body. The researchers were able to show for the first time how the main structural protein of LDL binds to its receptor – a process that starts the clearing of LDL from the blood – and what happens when that process gets impaired.
The findings, published in Nature, further the understanding of how LDL contributes to heart disease, the world’s leading cause of death, and could open the door to personalising LDL-lowering treatments like statins to make them even more effective.
“LDL is one of the main drivers of cardiovascular disease which kills one person every 33 seconds, so if you want to understand your enemy, you want to know what it looks like,” said Alan Remaley, MD, PhD, co-senior author on the study who runs the Lipoprotein Metabolism Laboratory at NIH’s National Heart, Lung, and Blood Institute.
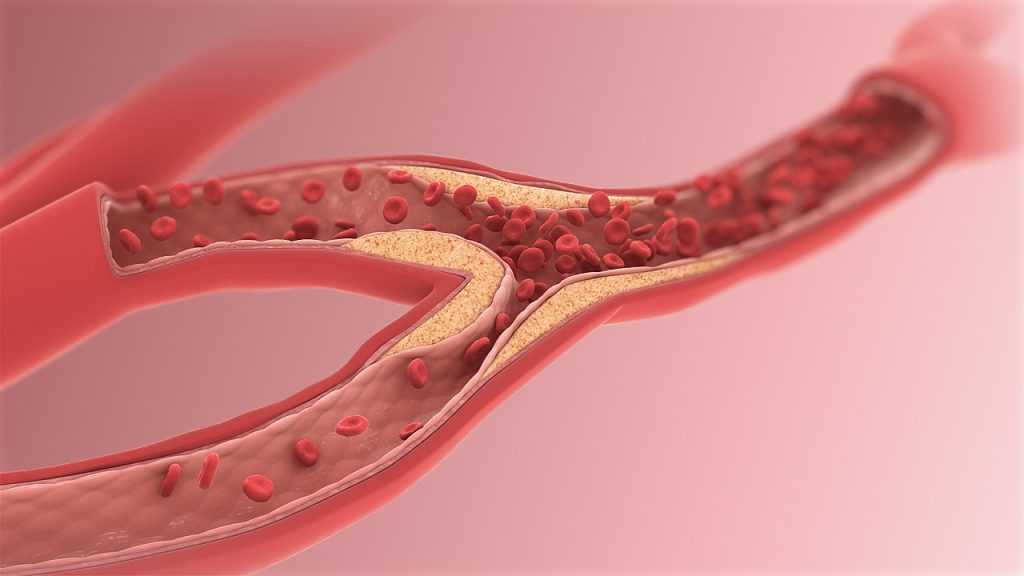
Until now scientists have been unable to visualise the structure of LDL, specifically what happens when it links up with its receptor, a protein known as LDLR. Typically, when LDL binds to LDLR, the process of clearing LDL from the blood begins. But genetic mutations can prevent that work, causing LDL to build up in the blood and get deposited into the arteries as plaque, which can lead to atherosclerosis, a precursor for heart disease.
In the new study, the researchers were able to use high-end technology to get a view of what’s happening at a critical stage of that process and see LDL in a new light.
“LDL is enormous and varies in size, making it very complex,” explained Joseph Marcotrigiano, PhD, chief of the Structural Virology Section in the Laboratory of Infectious Diseases at NIH’s National Institute of Allergy and Infectious Diseases and co-senior author on the study. “No one’s ever gotten to the resolution we have. We could see so much detail and start to tease apart how it works in the body.”
Using cryo-electron microscopy, the researchers were able to see the entirety of the structural protein of LDL when it bound to LDLR. Then, with AI-driven protein prediction software, they were able to model the structure and locate the known genetic mutations that result in increased LDL.
The researchers found that many of the mutations that mapped to the location where LDL and LDLR connected, were associated with familial hypercholesterolaemia (FH). FH is marked by defects in how the body uptakes LDL into its cells, and people with it have extremely high levels of LDL and can have heart attacks at a very young age. They found that FH-associated variants tended to cluster in particular regions on LDL.
The study findings could open new avenues to develop targeted therapies aimed at correcting these kinds of dysfunctional interactions caused by mutations. But, as importantly, the researchers said, they could also help people who do not have genetic mutations, but who have high cholesterol and are on statins, which lower LDL by increasing LDLR in cells. By knowing precisely where and how LDLR binds to LDL, the researchers say they may now be able to target those connection points to design new drugs for lowering LDL from the blood.





