Younger Children at Greater Risk for a Postoperative Knee Surgery Complication
New research published in Knee Surgery, Sports Traumatology, Arthroscopy has shown that younger age is associated with increased risk of osteochondritis dissecans, a serious complication arising from surgery to correct misshapen knee cartilage.
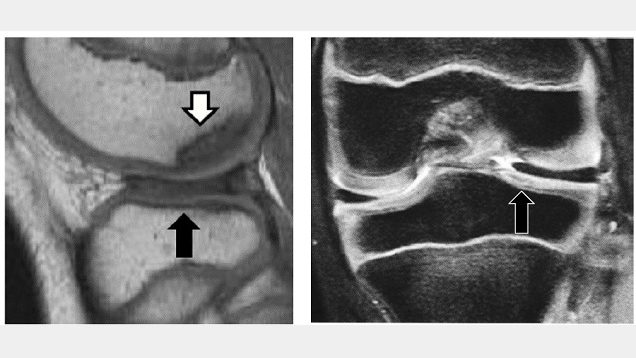
Growing pains are common in maturing children, but sometimes this growth can be irregular and cause injury. Discoid lateral meniscus (DLM), a misshapen knee cartilage, is one such occurrence that can degenerate into osteochondritis dissecans, a joint disorder where the bone and joint begin to separate from the rest of the bones. It has been reported that osteochondritis dissecans of the femoral condyle occurs in approximately 14.5% of cases of DLM, but there has been little analysis of its treatment to date.
Dr Ken Iida and Specially Appointed Professor Yusuke Hashimoto’s team at Osaka Metropolitan University’s Graduate School of Medicine analysed the incidence of post-surgery osteochondritis dissecans. This analysis consisted of two groups, a pre-osteochondritis group with DLM and osteochondritis dissecans of the outer femoral epicondyle, and a non-osteochondritis dissecans DLM group. They studied 95 cases of DLM patients under the age of 15 who underwent surgery between 2003 and 2017 and had five years of post-surgery records. There were 15 cases in the pre-osteochondritis dissecans group and 80 non-osteochondritis dissecans cases.
Their analysis found that the surgical results for osteochondritis dissecans were good in pre-osteochondritis cases, but 28.5% had a recurrence of the joint disorder. In the non-osteochondritis dissecans group, 8.8% were diagnosed with the disorder after surgery. Additionally, age was found to be a risk factor for relapse or post-surgical osteochondritis dissecans, and surgery on patients ages 9 and under was also involved in the occurrence of osteochondritis dissecans.
“Patients with DLM accompanied by osteochondritis dissecans of the femoral condyle often have difficulty in deciding on a treatment method,” Dr Iida explained. “Based on the results of this study, we believe for patients ages 9 years or younger, it is necessary to consider conservative treatment methods rather than immediate surgery.”
Source: Osaka Metropolitan University


