Noble Intentions: Xenon Gas might Protect against Alzheimer’s
Most treatments being pursued today to protect against Alzheimer’s disease focus on amyloid plaques and tau tangles that accumulate in the brain, but new research from Mass General Brigham and Washington University School of Medicine in St. Louis points to a novel – and noble – approach: using xenon gas. The study found that xenon gas inhalation suppressed neuroinflammation, reduced brain atrophy, and increased protective neuronal states in mouse models of Alzheimer’s disease. Results are published in Science Translational Medicine, and a phase 1 clinical trial of the treatment in healthy volunteers will begin in early 2025.
“It is a very novel discovery showing that simply inhaling an inert gas can have such a profound neuroprotective effect,” said senior and co-corresponding author Oleg Butovsky, PhD, at Brigham and Women’s Hospital (BWH). “One of the main limitations in the field of Alzheimer’s disease research and treatment is that it is extremely difficult to design medications that can pass the blood-brain barrier – but senon gas does. We look forward to seeing this novel approach tested in humans.”
“It is exciting that in both animal models that model different aspects of Alzheimer’s disease, amyloid pathology in one model and tau pathology in another model, that Xenon had protective effects in both situations,” said senior and co-corresponding author David M. Holtzman, MD, from Washington University School of Medicine in St. Louis.
The causes of Alzheimer’s disease are not fully understood; there is currently no cure, and more effective treatments are desperately needed. Characterised by protein buildups in the brain, including tau and amyloid, Alzheimer’s disease disrupts nerve cell communication and causes progressive brain abnormalities that lead to neuronal damage and ultimately to death. Microglia, the brain’s primary and most prominent immune cells, act as ‘first responders’ when something goes awry in the brain, and they play a key role in regulating brain function in all phases of development. Microglial dysregulation is a key component of Alzheimer’s disease. Butovsky’s lab previously designed a way to study how microglia respond to neurodegeneration and confirmed that a specific phenotype of microglia can be modulated in a way that is protective in Alzheimer’s disease.
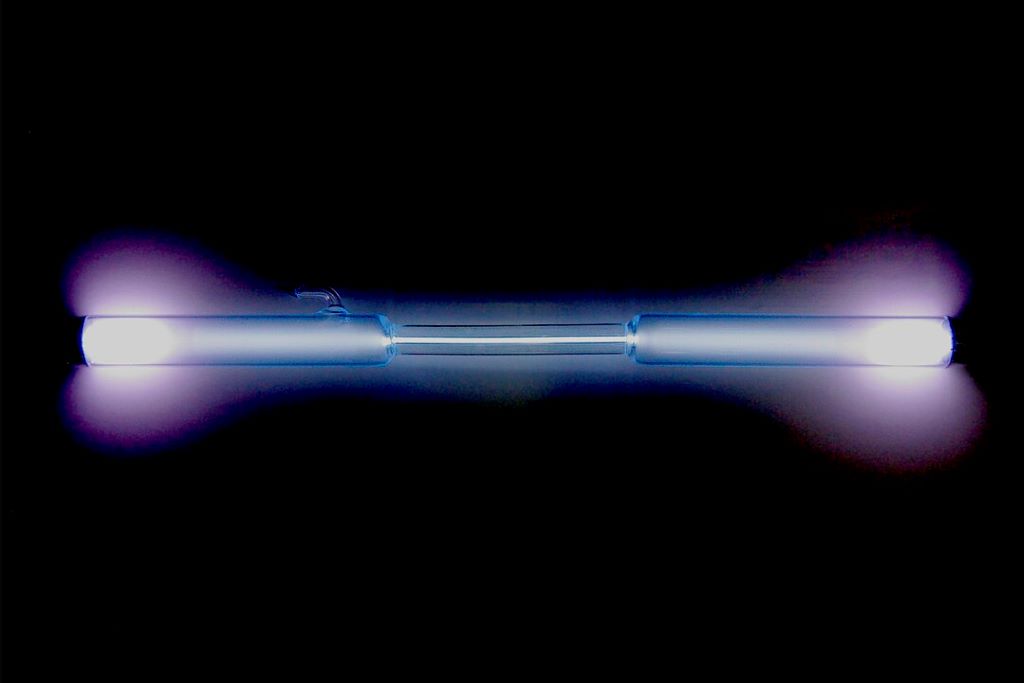
In this study, mouse models of Alzheimer’s disease were treated with xenon gas that has been used in human medicine as an anesthetic and as a neuroprotectant for treating brain injuries. Xenon gas penetrates the blood-brain barrier, passing from the bloodstream directly into the fluid surrounding the brain. The team found that xenon gas inhalation reduced brain atrophy and neuroinflammation and improved nest-building behaviours in the Alzheimer’s disease mouse models. It also induced and increased a protective microglial response that is associated with clearing amyloid and improving cognition. Together, these findings identify the promising potential of xenon inhalation as a therapeutic approach that could modify microglial activity and reduce neurodegeneration in Alzheimer’s disease.
The clinical trial at Brigham and Women’s Hospital, which will initially only enrol healthy volunteers, is set to begin in the next few months.
As early phases of the clinical trial get underway to establish safety and dosage, the research team plans to continue to study the mechanisms by which xenon gas achieves its effects in addition to its potential for treating other diseases such as multiple sclerosis, amyotrophic lateral sclerosis, and eye diseases that involve the loss of neurons. The team is also devising technologies to help use xenon gas more efficiently as well as potentially recycle it.
“If the clinical trial goes well, the opportunities for the use of Xenon gas are great,” said co-author Howard Weiner, MD, co-director of the Ann Romney Center for Neurologic Diseases at BWH and principal investigator of the upcoming clinical trial. “It could open the door to new treatments for helping patients with neurologic diseases.”
Source: Mass General Brigham


