Face Masks for Kids Slow Aerosol Spread, Especially from Sneezing

In a new study published in Pediatric Investigation, researchers demonstrate that face masks reduce the release of exhaled particles when used by school-aged children, helping to slow the spread of various respiratory viruses. While there was little difference between no protection and masking in exhaled particles from breathing, sneezing saw a significant reduction in the number of particles produced.
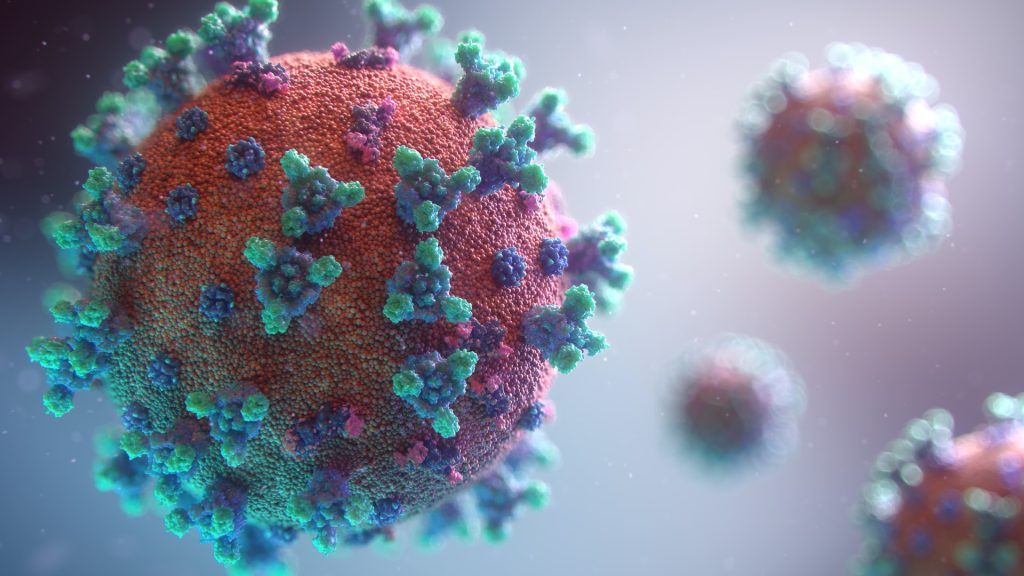
Respiratory viruses, including SARS-CoV-2, are transmitted via respiratory droplets and aerosols generated by all activities that involve exhalation, including tidal breathing, speaking, singing, coughing, and sneezing. Droplets, large particles subject to gravitational forces, are rapidly deposited from air and form fomites on surfaces. Aerosols, fine solid or liquid particles which remain suspended in the air, can travel long distances (> 6m) and reach high concentrations in poorly-ventilated areas. The relative contribution of the various modes of infection (direct contact, indirect contact via fomite, large droplet, or aerosol) for various respiratory viruses is difficult to determine, but survival of infectious viruses has been demonstrated in aerosols.
For the study, 23 healthy children were asked to perform activities that ranged in intensity (breathe quietly, speak, sing, cough, and sneeze) while wearing no mask, a cloth mask, or a surgical mask.
The production of exhaled particles that were 5μm or smaller, which is the dominant mode of transmission of many respiratory viruses, increased with coughing and sneezing. Face masks, especially surgical face masks, effectively reduced the release of these and other sized particles.
“Understanding the factors that affect respiratory particle emission can guide public health measures to prevent the spread of respiratory infections, which are a leading cause of death and hospitalisation among young children worldwide,” said corresponding author Peter P. Moschovis, MD, MPH, of Massachusetts General Hospital and Harvard Medical School.
Source: Wiley