High Cholesterol from Childhood Sedentary Time could be Reversed with Light Exercise

Increased sedentary time in childhood can raise cholesterol levels by two thirds as an adult, but a new study has found light physical activity may completely reverse the risks and is far more effective than moderate-to-vigorous physical activity.
The study was published in The Journal of Clinical Endocrinology & Metabolism. Researchers used data from the University of Bristol study Children of the 90s (also known as the Avon Longitudinal Study of Parents and Children), which included 792 children aged 11 years who were followed up until the age of 24.
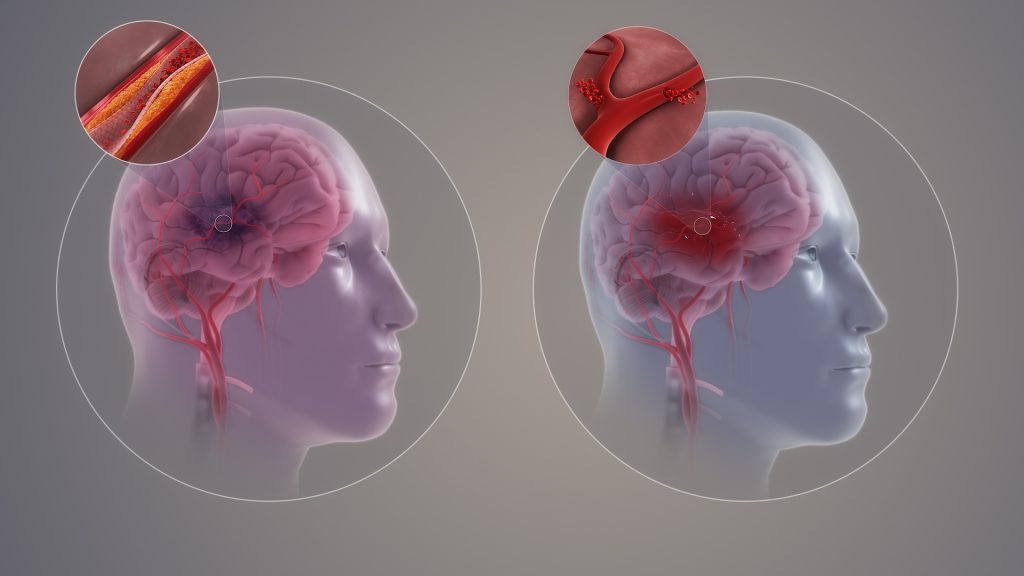
Results from this study found that accumulated sedentary time from childhood can increase cholesterol levels by two thirds (67%) by the time someone reaches their mid-twenties. Elevated cholesterol and dyslipidaemia from childhood and adolescence have been associated with premature death in the mid-forties and heart problems such as subclinical atherosclerosis and cardiac damage in the mid-twenties.
Healthy lifestyles are considered important in the prevention of dyslipidaemia and one of the primary ways of lowering cholesterol, apart from diet, is movement behaviour. For the first time, this study objectively examined the long-term effects of sedentary time, light physical activity, and moderate-to-vigorous physical activity on childhood cholesterol levels.
The World Health Organization currently recommends children and adolescents should accumulate on average 60 minutes of moderate-to-vigorous physical activity a day and reduce sedentary time but have limited guidelines for light physical activity. Yet this new study and other recent studies has found light physical activity – which includes exercises such as long walks, house chores, or slow dancing, swimming, or cycling – is up to five times more effective than moderate-to-vigorous physical activity at promoting healthy hearts and lowering inflammation in the young population.
Dr Andrew Agbaje from the University of Exeter led the study and said: “These findings emphasise the incredible health importance of light physical activity and shows it could be the key to preventing elevated cholesterol and dyslipidaemia from early life. We have evidence that light physical activity is considerably more effective than moderate-to-vigorous physical activity in this regard, and therefore it’s perhaps time the World Health Organization updated their guidelines on childhood exercise — and public health experts, paediatricians, and health policymakers encouraged more participation in light physical activity from childhood.”
During the research, accelerometer measures of sedentary time, light physical activity, and moderate-to-vigorous physical activity were collected at ages 11, 15, and 24 years. High-density lipoprotein cholesterol, low-density lipoprotein cholesterol, triglyceride, and total cholesterol were repeatedly measured at ages 15, 17, and 24 years. These children also had repeated measurement of dual-energy X-ray absorptiometry assessment of total body fat mass and muscle mass, as well as fasting blood glucose, insulin, and high sensitivity C-reactive protein, with smoking status, socio-economic status, and family history of cardiovascular disease.
During the 13-year follow-up, sedentary time increased from approximately six hours a day to nine hours a day. Light physical activity decreased from six hours a day to three hours a day while moderate-to-vigorous physical activity was relatively stable at around 50 minutes a day from childhood until young adulthood. The average increase in total cholesterol was 0.69 mmol/L. It was observed without any influence from body fat.
An average of four-and-a-half hours a day of light physical activity from childhood through young adulthood causally decreased total cholesterol by (-0.53 mmol/L), however, body fat mass could reduce the effect of light physical activity on total cholesterol by up to 6%. Approximately 50 minutes a day of moderate-to-vigorous physical activity from childhood was also associated with slightly reduced total cholesterol (-0.05 mmol/L), but total body fat mass decreased the effect of moderate-to-vigorous physical activity on total cholesterol by up to 48%. Importantly, the increase in fat mass neutralised the small effect of moderate-to-vigorous physical activity on total cholesterol.
Source: University of Exeter