Health in 2024: The Year in Fewer than 1000 Words

By Marcus Low and Adiel Ismail
From the NHI Act to major advances in HIV prevention, it has been another busy year in the world of healthcare. Spotlight editors Marcus Low and Adiel Ismail recap the year’s health developments and identify some key trends in fewer than 1000 words.
For a few weeks in June, it seemed that the surprising outcome of South Africa’s national and provincial elections would usher in far-reaching political and governance changes in the country. As it turns out, some significant changes did come, but not in the health sector.
Rather than a new broom, it was déjà vu as Dr Aaron Motsoaledi returned as Minister of Health – he was previously in the position from 2009 to 2019. In both Gauteng and KwaZulu-Natal – the country’s most populous provinces – ANC MECs for health from before the elections kept their jobs. The ANC garnered well under 50% of the votes in both of those provinces and nationally and accordingly had little choice but to form national and provincial coalitions.
To be fair, five of the nine MECs appointed after the elections were new, but these changes were mainly in the less populous provinces.

Policy-wise, the trajectory also remains much as it was a year ago. Two weeks before the elections, President Cyril Ramaphosa signed the National Health Insurance (NHI) Act into law (though most of it has not yet been promulgated). While Ramaphosa has since then asked Business Unity South Africa (BUSA), the country’s largest employer association, for new input on NHI and while talk of mandatory medical scheme cover had a moment in the headlines, there is no solid evidence that the ANC is open to changing course – if anything, Motsoaledi has doubled-down in the face of criticism. The Act is being challenged in various court cases.
The sense of discord in healthcare circles was further deepened in August when several organisations distanced themselves from Ramaphosa’s updated Presidential Health Compact. The South African Medical Association, the South African Health Professionals Collaboration—comprising nine associations representing over 25 000 public and private healthcare workers—and BUSA all declined to sign the accord. BUSA accused government of “unilaterally” amending the compact “transforming its original intent and objectives into an explicit pledge of support for the NHI Act”.
Away from these reforms, a trend of health budgets shrinking year-on-year in real terms continued this year. This funding crunch, together with well-documented shortages of healthcare workers, has meant that even well-run provincial health departments are having to make impossible trade-offs – that while governance in several provincial health departments remains chronically dysfunctional. This was underlined by a landmark report published in July that, among others, highlighted leadership instability, lack of transparency, insufficient accountability mechanisms, and pervasive corruption. New reports from the Auditor General also didn’t paint a pretty picture.
Gauteng health has again been in the headlines for the wrong reasons. The provision of cancer services in the province remains mired in controversy as the year comes to an end, with plans to outsource some radiation services to the private sector apparently having stalled, despite the health department having the money for it. A deal between the department and Wits University was also inexplicably derailed. With high vacancy rates, serious questions over senior appointments, reports of corruption at Thembisa Hospital, and much more, it seems that, if anything, governance in the province has gotten even worse this year.
In a precedent-setting inquest ruling in July, Judge Mmonoa Teffo found that the deaths of nine people moved from Life Esidimeni facilities to understaffed and under-equipped NGOs “were negligently caused by the conduct of” former Health MEC Qedani Mahlangu and former head of the provincial health department’s mental health directorate Dr Makgabo Manamela.
Outside our borders, Donald Trump’s election victory in the United States is set to have far-reaching consequences. A return of the Global Gag Rule seems likely, as does major changes to the Food and Drug Administration, the President’s Emergency Plan for AIDS Relief, and the National Institutes of Health – the latter funds much HIV and TB research in South Africa.
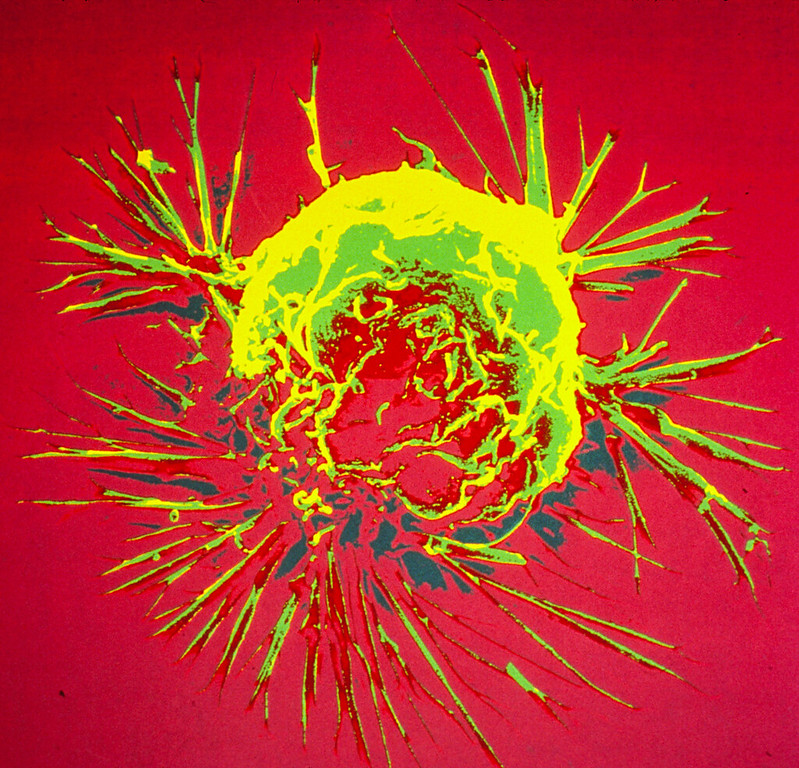
Away from politics and governance, the biggest HIV news of the year came in late June when it was announced that an injection administered every six months was extremely effective at preventing HIV infection. It will likely be several years before the jab becomes widely available in South Africa.

Another jab that provides two months of protection per shot is already available here, but only to a small number of people participating in implementation studies.
It is estimated that around 50 000 people died of HIV related causes in South Africa in 2023 and roughly 150 000 were newly infected with the virus (reliable estimates for 2024 will only be available in 2025). A worrying one in four people living with HIV were not on treatment in 2023. There was an estimated 56 000 TB deaths and around 270 000 people fell ill with the disease. While these HIV and TB numbers have come down dramatically over the last decade, they remain very high compared to most other countries.
There are some concerns that a new TB prevention policy published in 2023 is not being universally implemented. We have however been doing more TB tests, even while TB cases are declining – as we have argued, this is as it should be. Also positive, is that a massive trial of an TB vaccine kicked off in South Africa this year.
With both TB and HIV, South Africa is making progress too slowly, but we are at least trending in the right direction. With non-communicable diseases such as diabetes, there are unfortunately signs that things are getting worse. As we explained in one of our special briefings this year, our diabetes data in South Africa isn’t great, but the little we have painted a worrying picture. As expected, access to breakthrough new diabetes and weight loss medicines remained severely constrained this year, largely due to high prices and limited supply.
Ultimately then, at the end of 2024, South Africa is still faced with chronic healthcare worker shortages, severe governance problems in several provinces, and major uncertainties over NHI – all while HIV and TB remains major public health challenges, though a shift toward non-communicable diseases is clearly underway.
Republished from Spotlight under a Creative Commons licence.