The Micromort: A Simple Way to Convey Mortality Risk

When dealing with risks, the often-used metric of “deaths per 100 000 population” can be a bit unwieldy, especially when explaining risk to patients. During the COVID pandemic, this became something of a problem when trying to convey the risks of vaccination to the general public. Many felt that the risk of adverse effects outweighed the protection that the vaccination conferred against the coronavirus.
But there is a different, more approachable metric – in 1979, Ronald A. Howard introduced the ‘micromort’ – defined as one chance of death in a million. One in a million is about the same odds as flipping a coin 20 times a row and getting the same result.
Though its name is sure to make some people giggle, the micromort is commonly used in actuarial sciences and decision analyses to quantify the risk of death per unit of exposure to a risk factor or event (Howard, 1980). micromorts have the advantage of being easier to interpret and comprehend than abstract numerical figures, and have been used to convey risks associated with surgical operations and medical treatments.
For example, the mortality risk of general anaesthesia is 10 micromorts per procedure (ie, a 0.001% chance of dying), which is comparable to the mortality risk of an experienced skydiver takes when doing a parachute jump. Chronic cigarette smoking reduces adult life expectancy by 6.5 years on average; said differently, averaged over a lifetime, smoking reduces life expectancy by 7 micromorts per day (3.5 hours per day) (Shaw et al., 2000).
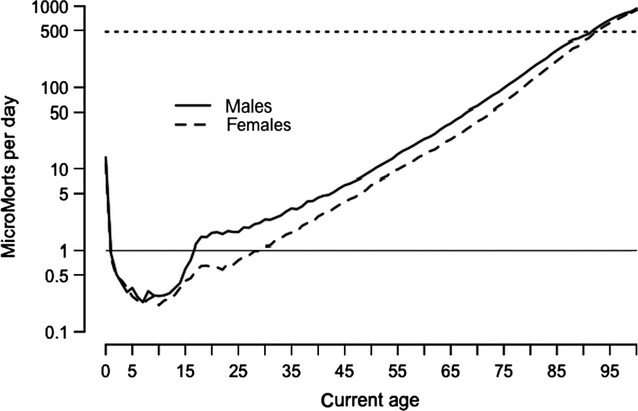
Simply being being alive carries a risk in itself: it is highest on the first day of lift at around 500 micromorts, drops rapidly in childhood and then increases steadily throughout adult life until the 90s, when each day is as risky as that person’s first day.
Perhaps unsurprisingly, one UK estimate showed that travelling by motorbike carries the highest risk of death at 9.6km for each MicroMort. Travelling by car is far safer at 400km per MicroMort. But somewhat counterintuitively, walking is not much safer than travelling by motorbike: hitting the pavement results in one MicroMort per 27.2km walked. This can be partly explained by the greater amount of time spent walking and exposed to environmental hazards such as traffic, air pollution, crime and so on.
The concept of micromorts can also be applied to pregnancies and risks to the foetus. The risk per unit due to stillbirth is only about 19 or 3710 micromorts when drinking 5 units/week throughout pregnancy. For low risk women in the UK, planned first birth at home carries an additional 843 (-200 to 2620) micromorts compared with in hospital, and planned vaginal breech birth an additional 5870 (-4400 to 18 500), compared with planned caesarean. By contrast, the risk from the mother eating a serving of unpasteurised cheese, is negligible at 0.00026 micromorts (Hickson et al., 2020).




