How Bacteria Hijack Pain Neurons to Cause Meningitis
A new study details the step-by-step cascade that allows bacteria to break through the brain’s protective layers, the meninges, and cause meningitis, a highly fatal disease. Published in Nature, the mouse-based research shows that bacteria exploit nerve cells in the meninges to suppress the immune response and allow the infection to spread into the brain.
“We’ve identified a neuroimmune axis at the protective borders of the brain that is hijacked by bacteria to cause infection – a clever manoeuvre that ensures bacterial survival and leads to widespread disease,” said study senior author Isaac Chiu, associate professor of immunology in the Blavatnik Institute at Harvard Medical School.
The study identifies two central players in this molecular chain of events that leads to infection – a chemical released by nerve cells and an immune cell receptor blocked by the chemical. The study experiments show that blocking either one can interrupt the cascade and thwart the bacterial invasion.
If replicated through further research, the new findings could lead to much-needed therapies for this hard-to-treat condition that often leaves those who survive with serious neurologic damage.
Such treatments would target the critical early steps of infection before bacteria can spread deep into the brain.
“The meninges are the final tissue barrier before pathogens enter the brain, so we have to focus our treatment efforts on what happens at this border tissue,” said study first author Felipe Pinho-Ribeiro, a former post-doctoral researcher in the Chiu lab, now an assistant professor at Washington University in St. Louis.
A recalcitrant disease in need of new treatments
More than 1.2 million cases of bacterial meningitis occur globally each year, according to the US Centers for Disease Control and Prevention. Untreated, it kills seven out of 10 people who contract it. Treatment can reduce mortality to three in 10. However, among those who survive, one in five experience serious consequences, including hearing or vision loss, seizures, chronic headache, and other neurological problems.
The meninges are three membranes that lie atop one another, wrapping the brain and spinal cord to shield the central nervous system from injury, damage, and infection. The dura mater, outermost of the three layers, contains pain neurons that detect signals. Such signals could come in the form of mechanical pressure: blunt force from impact or toxins that make their way into the central nervous system through the bloodstream. The researchers focused on the dura mater as the site of initial interaction between bacteria and protective border tissue.
Recent research has revealed that the dura mater also harbours a wealth of immune cells, and that immune cells and nerve cells reside right next to each other – a clue that captured Chiu’s and Pinho-Ribeiro’s attention.
“When it comes to meningitis, most of the research so far has focused on analysing brain responses, but responses in the meninges – the barrier tissue where infection begins – have remained understudied,” Ribeiro said.
What exactly happens in the meninges when bacteria invade? How do they interact with the immune cells residing there? These questions remain poorly understood, the researchers said.
How bacteria break through the brain’s protective layers
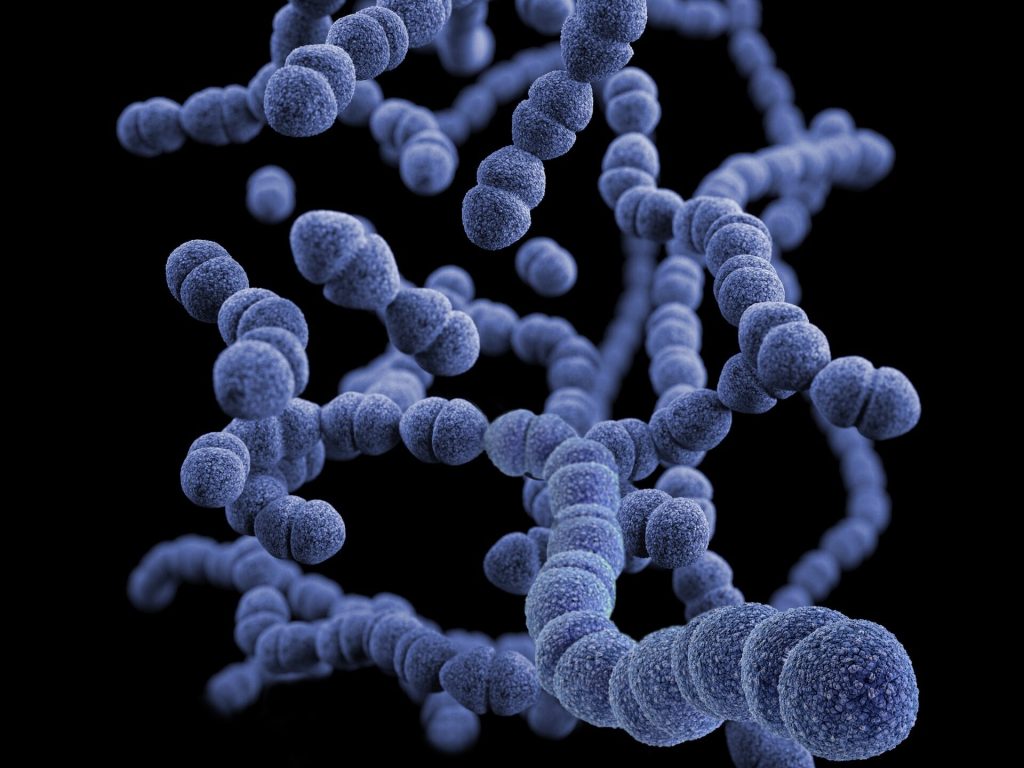
In this particular study, the researchers focused on two pathogens – Streptococcus pneumoniae and Streptococcus agalactiae, leading causes of bacterial meningitis in humans. In a series of experiments, the team found that when bacteria reach the meninges, the pathogens trigger a chain of events that culminates in disseminated infection.
First, researchers found that bacteria release a toxin that activates pain neurons in the meninges. The activation of pain neurons by bacterial toxins, the researchers noted, could explain the severe, intense headache that is a hallmark of meningitis. Next, the activated neurons release a signalling chemical called CGRP. CGRP attaches to an immune-cell receptor called RAMP1. RAMP1 is particularly abundant on the surface of immune cells called macrophages.
Once the chemical engages the receptor, the immune cell is effectively disabled. Under normal conditions, as soon as macrophages detect the presence of bacteria, they spring into action to attack, destroy, and engulf them. Macrophages also send distress signals to other immune cells to provide a second line of defence. The team’s experiments showed that when CGRP gets released and attaches to the RAMP1 receptor on macrophages, it prevented these immune cells from recruiting help from fellow immune cells. As a result, the bacteria proliferated and caused widespread infection.
To confirm that the bacterially induced activation of pain neurons was the critical first step in disabling the brain’s defences, the researchers checked what would happen to infected mice lacking pain neurons.
Mice without pain neurons developed less severe brain infections when infected with two types of bacteria known to cause meningitis. The meninges of these mice, the experiments showed, had high levels of immune cells to combat the bacteria. By contrast, the meninges of mice with intact pain neurons showed meagre immune responses and far fewer activated immune cells, demonstrating that neurons get hijacked by bacteria to subvert immune protection.
To confirm that CGRP was, indeed, the activating signal, researchers compared the levels of CGRP in meningeal tissue from infected mice with intact pain neurons and meningeal tissue from mice lacking pain neurons. The brain cells of mice lacking pain neurons had barely detectable levels of CGRP and few signs of bacterial presence. By contrast, meningeal cells of infected mice with intact pain neurons showed markedly elevated levels of both CGRP and more bacteria.
In another experiment, the researchers used a chemical to block the RAMP1 receptor, preventing it from communicating with CGRP, the chemical released by activated pain neurons. The RAMP1 blocker worked both as preventive treatment before infection and as a treatment once infection had occurred.
Mice pretreated with RAMP1 blockers showed reduced bacterial presence in the meninges. Likewise, mice that received RAMP1 blockers several hours after infection and regularly thereafter had milder symptoms and were more capable of clearing bacteria, compared with untreated animals.
A path to new treatments
The experiments suggest drugs that block either CGRP or RAMP1 could allow immune cells to do their job properly and increase the brain’s border defenses.
Compounds that block CGRP and RAMP1 are found in widely used drugs to treat migraine, a condition believed to originate in the top meningeal layer, the dura mater. Could these compounds become the basis for new medicines to treat meningitis? It’s a question the researchers say merits further investigation.
One line of future research could examine whether CGRP and RAMP1 blockers could be used in conjunction with antibiotics to treat meningitis and augment protection.
“Anything we find that could impact treatment of meningitis during the earliest stages of infection before the disease escalates and spreads could be helpful either to decrease mortality or minimize the subsequent damage,” Pinho-Ribeiro said.
More broadly, the direct physical contact between immune cells and nerve cells in the meninges offers tantalizing new avenues for research.
“There has to be an evolutionary reason why macrophages and pain neurons reside so closely together,” Chiu said. “With our study, we’ve gleaned what happens in the setting of bacterial infection, but beyond that, how do they interact during viral infection, in the presence of tumour cells, or the setting of brain injury? These are all important and fascinating future questions.”
Source: Harvard Medical School





