Experimental Drug may Prevent Diabetic Vision Loss
Researchers at Wilmer Eye Institute, Johns Hopkins Medicine say they have evidence that an experimental drug may prevent or slow vision loss in people with diabetes. The results are from a study published in the Journal of Clinical Investigation, that used mouse models as well as human retinal organoids and eye cell lines.
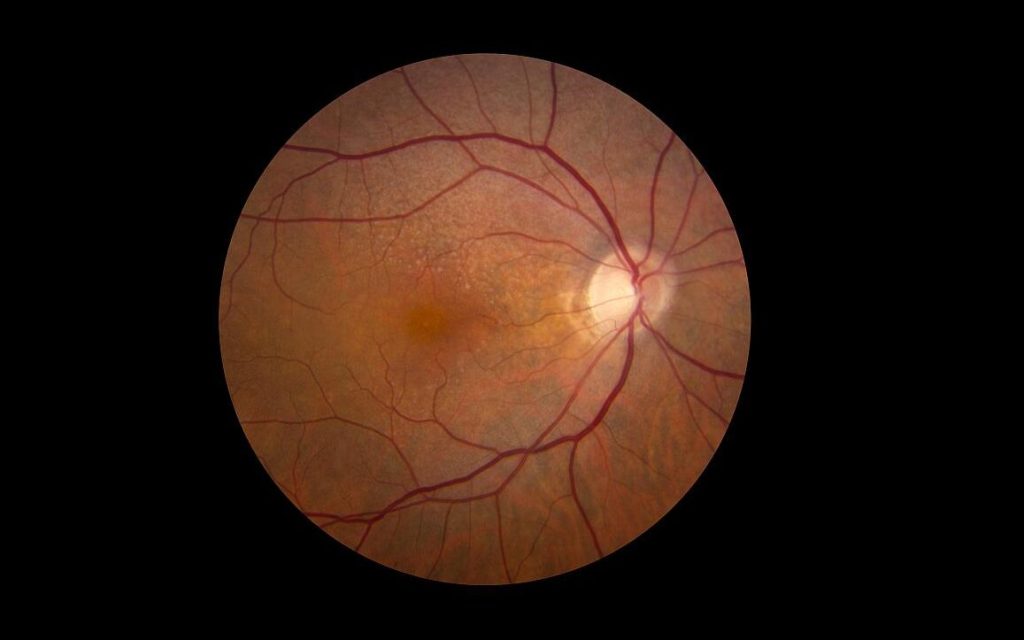
The team focused on models of two common diabetic eye conditions: proliferative diabetic retinopathy and diabetic macular enema, both of which affect the retina, the light-sensing tissue at the back of the eye that also transmits vision signals to the brain. In proliferative diabetic retinopathy, new blood vessels overgrow on the retina’s surface, causing bleeding or retinal detachments and profound vision loss. In diabetic macular enema, blood vessels in the eye leak fluid, leading to swelling of the central retina, damaging the retinal cells responsible for central vision.
Results of the study show that a compound called 32-134D, previously shown to slow liver tumour growth in mice, prevented diabetic retinal vascular disease by decreasing levels of a protein called HIF, or hypoxia-inducible factor. Doses of 32-134D also appeared to be safer than another treatment that also targets HIF and is under investigation to treat diabetic eye disease.
Current treatment for both proliferative diabetic retinopathy and diabetic macular enema includes eye injections with anti-vascular endothelial growth factor (anti-VEGF) therapies. Anti-VEGF therapies can halt the growth and leakiness of blood vessels in the retina in patients with diabetes. However, these treatments aren’t effective for many patients, and may cause side effects with prolonged use, such as increased internal eye pressure or eye tissue damage.
Study author Akrit Sodhi, MD, PhD, says that in general, the idea of inhibiting HIF, a fundamental protein in the body, has raised concerns about toxicity to many tissues and organs. But when his team screened a library of HIF inhibitor drugs and conducted extensive testing, “We came to find that the drug examined in this study, 32-134D, was remarkably well tolerated in the eyes and effectively reduced HIF levels in diseased eyes,” says Sodhi.
HIF, a type of protein known as a transcription factor, has the ability to switch certain genes, including vascular endothelial growth factor (VEGF), on or off throughout the body. In the eye, elevated levels of HIF cause genes like VEGF to increase blood vessel production and leakiness in the retina, contributing to vision loss.
To test 32-134D, researchers dosed multiple types of human retinal cell lines associated with the expression of proteins that promote blood vessel production and leakiness. When they measured genes regulated by HIF in cells treated with 32-134D, they found that their expression had returned to near-normal levels, which is enough to halt new blood vessel creation and maintain blood vessels’ structural integrity.
Researchers also tested 32-134D in two different adult mouse models of diabetic eye disease. In both models, injections were administered into the eye. Five days post-injection, the researchers observed diminished levels of HIF, and also saw that the drug effectively inhibited the creation of new blood vessels or blocked vessel leakage, therefore slowing progression of the animals’ eye disease. Sodhi and his team said they also were surprised to find that 32-134D lasted in the retina at active levels for about 12 days following a single injection without causing retinal cell death or tissue wasting.
“This paper highlights how inhibiting HIF with 32-134D is not just a potentially effective therapeutic approach, but a safe one, too,” says Sodhi. “People facing diabetic eye disease and vision loss include our family members, friends, co-workers – this is a disease that impacts a large group of people. Having safer therapies is critical for this growing population of patients.”
Sodhi says that further studies in animal models are needed before moving to clinical trials.
Source: Johns Hopkins Medicine