Metastasis and Atherosclerosis Share an Underlying Mechanism
Researchers have identified a key signalling molecule for cancer metastasis. one which is already known for its involvement in atherosclerosis, suggesting a possible treatment approach for both diseases simultaneously. The discovery was published in the International Journal of Cancer.
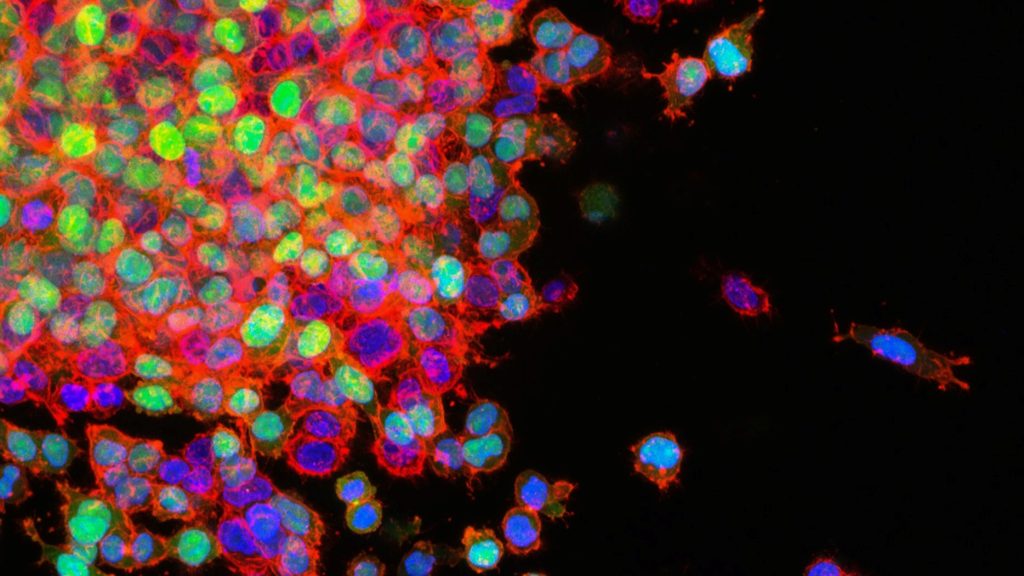
In order to become malignant, metastasising cancer, tumour cells undergo a series of transformations involving interactions with the immune system. Growing evidence exists that in tumour progression to metastasis, inflammation of blood vessel-lining endothelial cells is a key process.
A team of researchers led by Professor Kyoko Hida at Hokkaido University have discovered that, in malignant tumours, endothelial cells accumulate low-density lipoprotein (LDL) and neutrophils. Neutrophils are immune suppressor cells which are known to contribute to tumour progression.
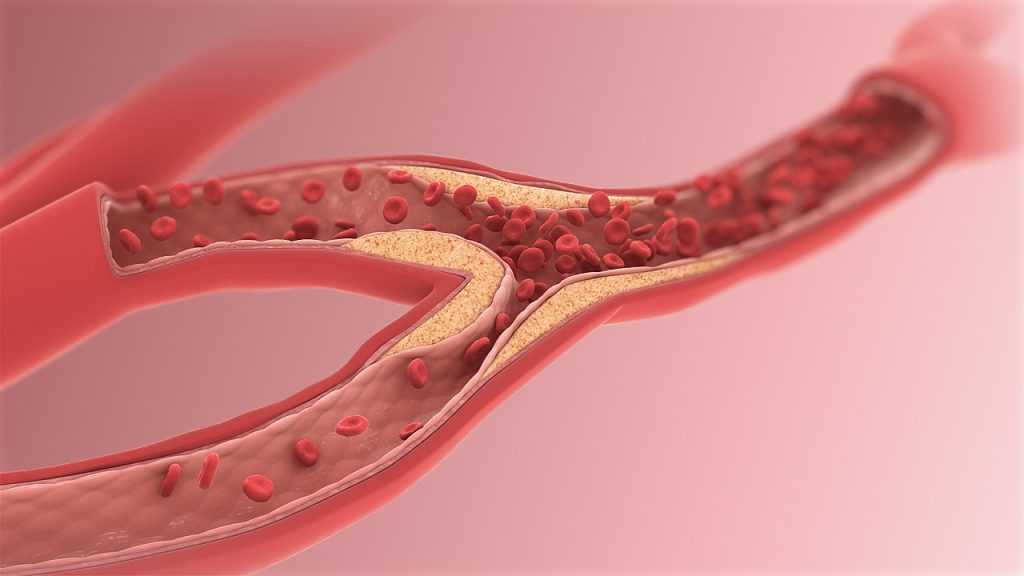
Previous work by the team had revealed that blood vessels in malignant tumorus expressed a high level of proteoglycans, and it is known that cancerous tissue is inflamed – similar to what is seen in atherosclerosis.
The research team showed that metastasising tumors, in contrast to non-metastasising ones, accumulate proteoglycan molecules; these, in turn, attach to and accumulate LDL to the walls of blood vessels, where it becomes oxidised. There are also high levels of its receptor, LOX-1, in the blood vessel-lining endothelial cells of metastasising tumours. This, they found, causes these cells to produce inflammation signals that attract neutrophils. Using a mouse model, they proved that the suppression of LOX-1 can significantly reduce tumour malignancy, and also that LOX-1 overexpression caused an increase in signalling molecules attracting neutrophils.
This sequence of interactions observed in malignant tumours is not novel: it occurs in atherosclerosis. “Atherosclerosis and cancer appear to be completely different diseases, but they share several common pathophysiological features in the blood vessels,” said Prof Hida.
Though some questions remain, especially on the mechanism of how neutrophils contribute to cancer malignancy, this study is the first to explicitly prove the mechanistic commonalities between cardiovascular disease and cancer progression and trace the mechanism involving LDL accumulation and LOX-1 expression in in vivo tumour tissue.
“Our present study focused on the importance of LOX-1 in endothelial cells as a common factor between cancer and atherosclerosis,” Prof Hida explained. “The presence of neutrophils in tumours is a telltale sign of tumor progression.”
The study also points to a promising approach for treating and preventing malignant cancer (and cardiovascular disease) by targeting neutrophil recruitment to endothelial cells. Prof Hida concluded: “The number of patients with cancer who die not of cancer, but of cardiovascular events, is increasing. Targeting the LOX-1/oxidised LDL axis might be a promising strategy for the treatment of the two diseases concomitantly.”
Source: Hokkaido University