It’s in the Mix: Certain Combinations of Pathogens Resist Antibiotics
A study has found that much higher doses of antibiotics are needed to eliminate a bacterial infection of the airways when certain other microbes are present. This helps explain why treatment often fails to treat respiratory infections in people with diseases such as cystic fibrosis.
The study’s researchers, whose findings are published in The ISME Journal, say that even a low level of one type of microbe in the airways can have a significant impact on the response of other microbes to antibiotics.
The results highlight the need to consider the interaction between different species of microbe when treating infections with antibiotics – and to adjust dosage accordingly.
“People with chronic infections often have co-infection with several pathogens, but the problem is we don’t take that into account in deciding how much of a particular antibiotic to treat them with. Our results might help explain why, in these people, the antibiotics just don’t work as well as they should,” said Thomas O’Brien, PhD candidate and co-first author.
Chronic bacterial infections such as those in the human airways are very difficult to cure using antibiotics. Although these types of infection are often associated with a single pathogenic species, the infection site is frequently co-colonised by a number of other microbes, most of which are not usually pathogenic in their own right.
Treatment options usually revolve around targeting the pathogen, and take little account of the co-habiting species. However, these treatments often fail to resolve the infection. Until now scientists have had little insight into why this is.
To get their results the team developed a simplified model of the human airways, containing artificial sputum designed to chemically resemble the real thing, packed with bacteria.
The model allowed them to grow a mixture of different microbes, including pathogens, in a stable way for weeks at a time. This is a novel approach, as usually one pathogen will rapidly outgrow the others and spoil the experiment. It enabled the researchers to replicate and study poly-microbial infections in the laboratory.
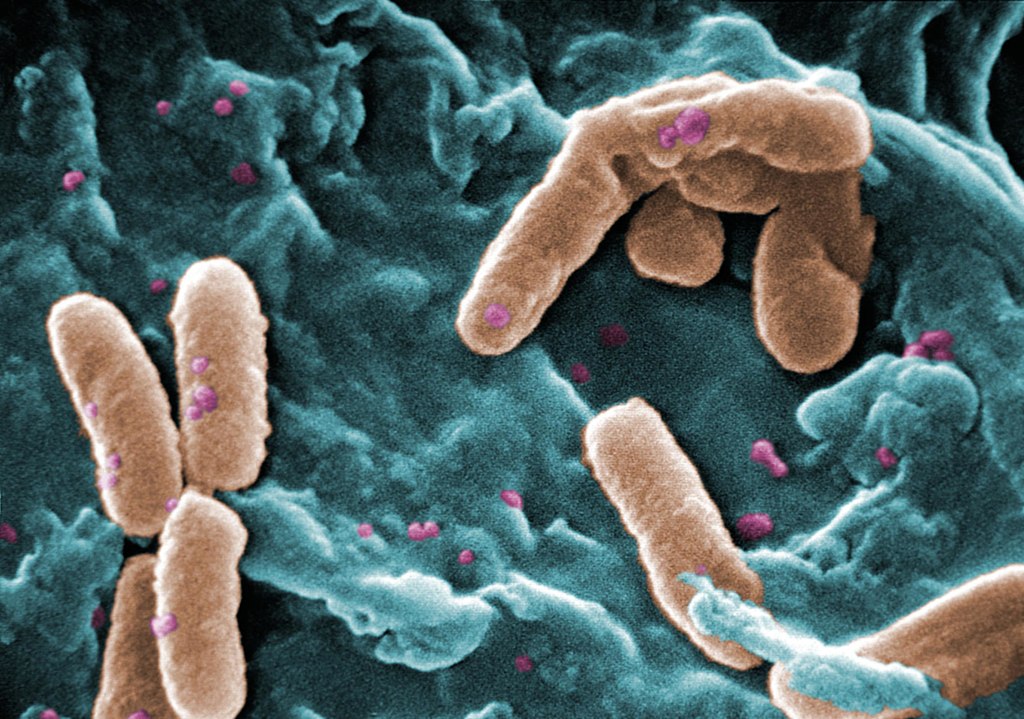
The three microbes used in the experiment were the bacteria Pseudomonas aeruginosa and Staphylococcus aureus, and the fungus Candida albicans – a combination often found in the airways of cystic fibrosis patients.
The researchers treated this microbial mix with colistin, which kills P. aeruginosa effectively. But when the other pathogens were present alongside P. aeruginosa, the antibiotic didn’t work.
“We were surprised to find that an antibiotic that we know should clear an infection of Pseudomonas effectively just didn’t work in our lab model when other bugs were present,” said Wendy Figueroa-Chavez at the University of Cambridge, joint first author of the paper.
The same effect happened when the microbial mix was treated with fusidic acid – an antibiotic that specifically targets Staphylococcus aureus, and with fluconazole, which specifically targets C. albicans.
The researchers found that significantly higher doses of each antibiotic were needed to kill bacteria when it was part of poly-microbial infection, compared to when no other pathogens were present.
“All three species-specific antibiotics were less effective against their target when three pathogens were present together,” said Professor Martin Welch at the University of Cambridge, senior author of the paper.
Currently, antibiotics are usually only lab tested against the targeted pathogen, to determine the lowest effective dose. But when the same dose is used to treat infection in a person it is often ineffective, and this study helps to explain why. The new model system will enable the effectiveness of potential new antibiotics to be tested against a mixture of microbe species together.
Poly-microbial infections are common in the airways of people with cystic fibrosis. Despite treatment with strong doses of antibiotics, these infections often persist long-term. Chronic infections of the airways in people with asthma and chronic obstructive pulmonary disorder (COPD) are also often poly-microbial.
Genetically analysing the Pseudomonas in their lab-grown mix, the researchers were able to pinpoint specific mutations that give rise to this antibiotic resistance. The mutations were found to arise more frequently when other pathogens were also present.
Comparison with the genetic code of 800 samples of Pseudomonas from around the world revealed that these mutations have also occurred in human patients who had been infected with Pseudomonas and treated with colistin.
“The problem is that as soon as you use an antibiotic to treat a microbial infection, the microbe will start to evolve resistance to that antibiotic. That’s what has happened since colistin started to be used in the early 1990’s. This is another reminder of the vital need to find new antibiotics to treat human infections,” said Prof Welch.
Source: University of Cambridge



