IBS Dietary Therapy Works Best with Certain Gut Microbiomes
People who respond well to the irritable bowel syndrome (IBS) dietary therapy of reduced fermentable carbs have an abundance of particular types of bacteria in their gut, reveals research published online in the journal Gut.
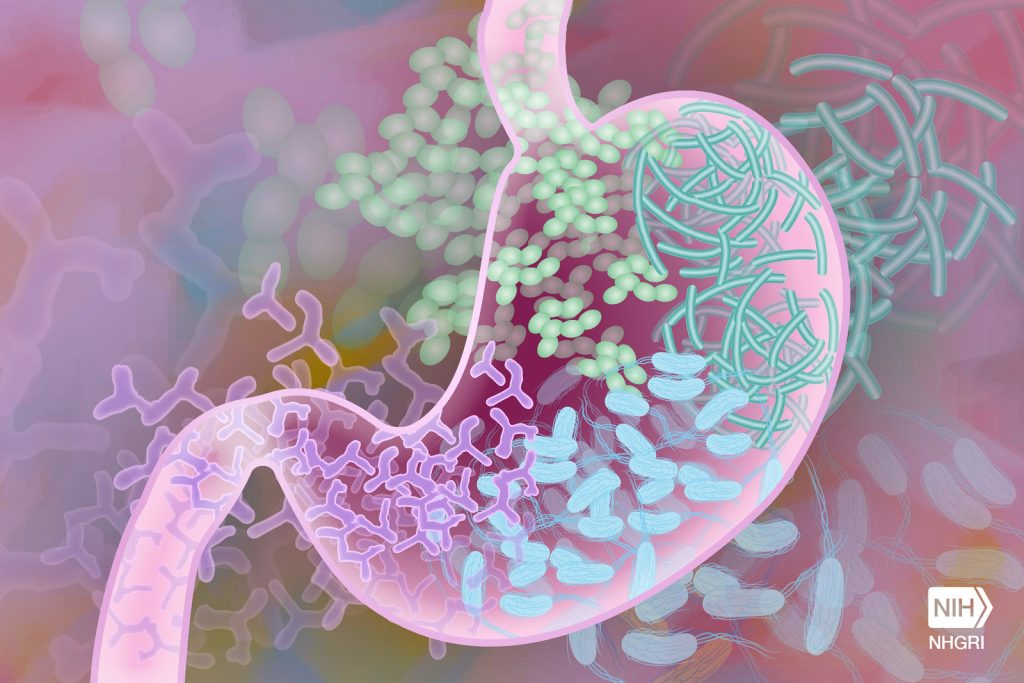
The composition of the gut microbiome is thought to have a major role in the development of IBS. Restricting fermentable carbs, found in many foods including wheat, onions, and milk, is usually recommended to ease symptoms, an approach known as the low FODMAP (fermentable oligo-, di-, mono-saccharides and polyols) diet. But why this diet works is not fully understood.
In a bid to fill this knowledge gap, the researchers analysed stool samples of 56 people with IBS and 56 people who lived with them, but without the condition, to identify the microbial profile and genes involved in converting food into active molecules while on their usual diet.
They then assessed the clinical response in 41 of these pairs after 4 weeks on the low FODMAP diet by reviewing their stool samples again.
Before adoption of the low FODMAP diet, analysis of the stool samples of those with IBS revealed two distinct microbial ‘signatures’, which the researchers referred to as ‘pathogenic-like’ (IBSP) and as ‘health-like’ (IBSH).
The pathogenic microbial signature was abundant in harmful Firmicutes sp, including known disease causing bacteria, such as C. difficile, C. sordellii and C. perfringens, but very low in beneficial Bacteroidetes species.
The lactic acid bacteria Streptococcus parasanguinis and Streptococcus timonensis that are usually found in the mouth were also abundant. And bacterial genes for amino acid and carbohydrate metabolism were overexpressed, which may explain the excess of some metabolites that are linked to IBS symptoms, say the researchers.
The healthy microbial signature of the other IBS patients was similar to that found in the comparison group (household members).
After 4 weeks on the low FODMAP diet, the microbiome of the comparison group and those with the healthy microbial profile stayed the same.
But the microbiome of those with the pathogenic profile became healthier, with an increase in Bacteroidetes, and a fall in Firmicutes species. And the bacterial genes involved in the metabolism of amino acids and carbs were no longer overexpressed.
In 3 out of 4 of IBS patients, symptoms improved. But the clinical response to the low FODMAP diet was greater in those with IBS and a pathogenic microbial signature than it was in those with IBS and a healthy microbial signature in their gut.
“The evidence associating diet, the microbiome and symptoms in [pathogenic IBS] is compelling, but studies following the introduction of candidate organisms into an animal model are needed to prove the relationship is causal,” the researchers cautioned.
Nevertheless, they suggest their findings could lead to a microbial signature to identify those who would respond best to a low FODMAP diet and better manage those who wouldn’t.
“If the bacteria represented in the [pathogenic] subtype are shown to play a pathogenic role in IBS, perhaps through their metabolic activity, this provides a target for new therapies and an intermediate [marker] by which to assess them,” they suggest.
In a linked editorial, Professor Peter Gibson and Dr Emma Halmos of Melbourne’s Monash University, describe the introduction and adoption of the FODMAP diet as “a major change in the management of patients with irritable bowel syndrome (IBS) towards integrated care.
But while “an effective symptomatic therapy, [it’s] one that carries risks associated with exacerbating disordered eating, challenging nutritional adequacy and putatively inducing dysbiotic gut microbiota,” they added.
They point out some limitations of the research, including that FODMAP intake was poorly assessed, fibre intake,which can also influence the microbiome wasn’t reported and patient drop-out reduced the power of the study.
Nevertheless, the authors concluded that “the beauty of [the study] is not in its definitive nature, but that it enables the creation of feasible innovative hypotheses that can be examined by focused studies. Perhaps the FODMAP diet is not just a symptomatic therapy.”
Source: BMJ