The Potential Dangers of ‘Harmless’ Herbal Supplements

While herbal supplements may be natural, they may not always be harmless. In Heart Rhythm Case Reports, doctors report on a patient who experienced dizziness and fainting and was diagnosed with a dangerous cardiac arrhythmia after taking hemp oil containing CBD and CBG and berberine supplements.
“More and more people are taking herbal supplements for their potential benefits. Yet their ‘natural’ character can be misleading, since these preparations can have serious adverse side effects on their own or if combined with other supplements or medications,” said Elise Bakelants, MD, Department of Cardiology, University Hospital of Geneva. “Their use should not be taken lightly, and dosing recommendations should always be respected.”
The reported case involves a 56-year-old woman who was admitted to the emergency department after experiencing dizziness and fainting without warning. She was diagnosed with a life-threatening cardiac arrhythmia after an ECG showed short runs of torsade de pointes, a rapid heartbeat originating in the ventricles, and a markedly prolonged QT interval, which means the heart’s electrical system takes longer than normal to recharge between beats.
Apart from low blood pressure, the patient’s physical examination and blood work were normal. The doctors were able to identify the cause as the herbal supplements she was taking to help her cope with a stressful work-life balance. She had started a regimen of six times the recommended dose of hemp oil four months earlier and had recently added berberine to the mix. All supplements were stopped during her hospital stay, resulting in a gradual decrease of her QT interval until it normalized after five days. At her three-month follow-up, she reported no new episodes of dizziness or fainting, and her ECG remained within normal range. With no other causative factors, her return to normal strongly validated that the diagnosis linked the supplements to the arrhythmia.
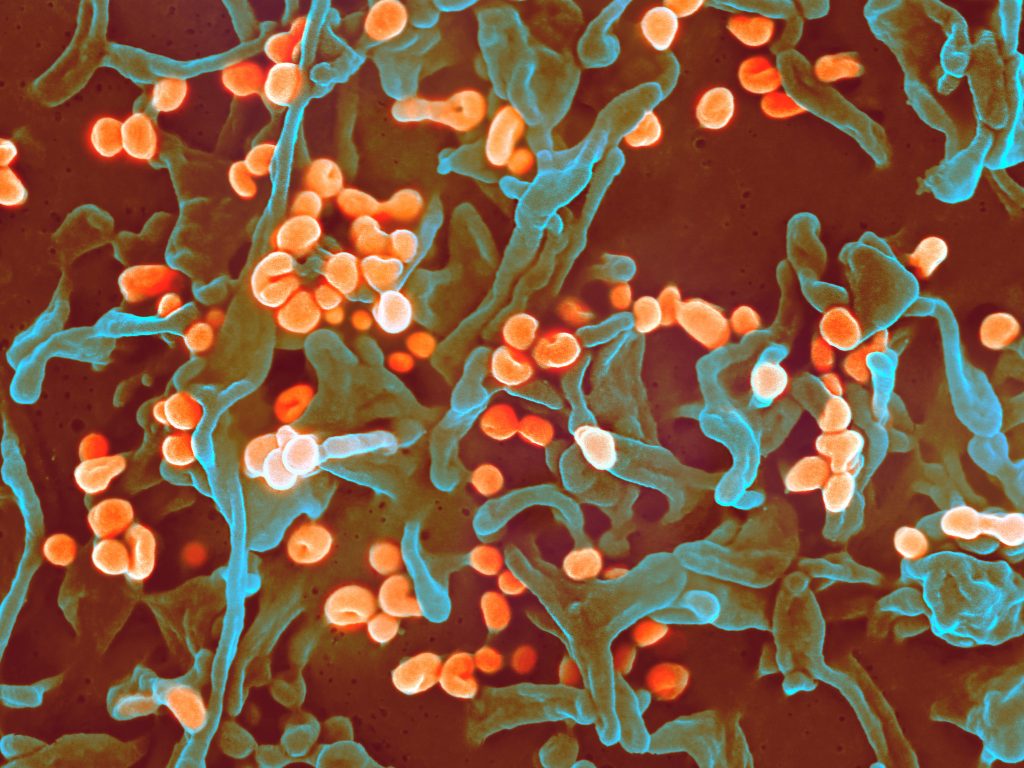
Herbal supplements has increased in popularity in recent years, especially those containing CBD (cannabidiol). Available without prescription, CBD has been shown to have anti-inflammatory, antiepileptic, analgesic, anxiolytic, antipsychotic, and immunomodulatory properties. Supplied as raw material or as ready-to-use products (eg, cosmetics, tobacco substitutes, scented oils), it does not contain THC (tetrahydrocannabinol), which causes the psychotropic effect of cannabis. Therefore, it is not subject to control by drug regulatory agencies. Berberine, found in the roots, rhizomes, and stem bark of many medicinal plants, is frequently used in traditional Chinese and ayurvedic medicine to treat infections, diarrhoea, type 2 diabetes, high cholesterol, and high blood pressure.
The e preparation of herbal supplements is largely unregulated and are widely perceived as safe. Exact composition can vary greatly from one distributor to another, and the pharmacodynamic and pharmacokinetic properties of these substances are not well known. Limited data are available regarding their effectiveness, toxicity, and potential for interactions. As a result, it is not always possible to foresee their negative consequences.
Dr Bakelants cautioned patients and physicians to be aware of possible side effects, respect dosing recommendations and consider possible interactions with other medications, particularly in patients with underlying cardiac disease or those already taking QT-prolonging medication.
Source: EurekAlert!