An Existing Cancer Drug Could Have a New Target: Cancer Cells’ ‘Fountain of Youth’

A team of scientists has found that ponatinib, an existing cancer drug could be repurposed to target a subset of cancers that currently lack targeted treatment options and is often associated with poor outcomes. Their findings are published in Nature Communications.
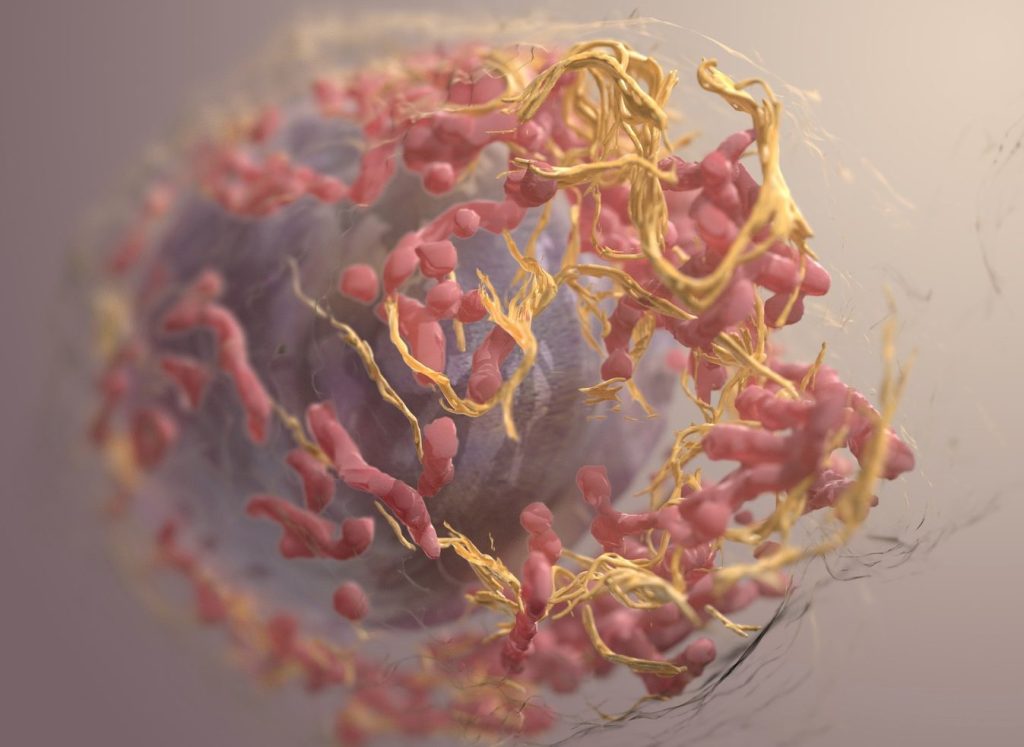
Cancerous cells have a ‘fountain of youth’ by continually lengthening telomeres, but some use a different mechanism called the alternative lengthening of telomeres (ALT). This subset makes up 15% of all cancers and is especially prevalent in aggressive tumours such as osteosarcoma and glioblastoma. The team, led by Nanyang Technological University, Singapore (NTU Singapore), showed that ponatinib, a cancer drug approved by the US Food and Drug Administration, blocks key steps in the ALT mechanism that leads it to fail.
The scientists found that ponatinib helped to shrink bone tumours (a type of ALT cancer) without causing weight loss, a common side effect associated with cancer drugs. In mice with tumours treated with ponatinib, they found a reduction in a biomarker for ALT cancer as compared to untreated mice.
The researchers say that the findings move them a step closer to developing a targeted therapeutic option for ALT cancers, which lack clinically approved targeted treatments to date.
Dr Maya Jeitany and a team of researchers from the NTU School of Biological Sciences, together with collaborators are seeking to address this unmet need.
Dr Jeitany, study lead and senior research fellow at NTU’s School of Biological Sciences, said: “A prominent feature of cancer is its ability to evade cell death and acquire indefinite replication – to stay immortal, in other words – which it can do through the alternative lengthening of telomeres (ALT) mechanism. While a sizeable portion of cancer cells depend on this mechanism, there is no clinically approved targeted therapy available.
“Through our study, we identified a novel signalling pathway in the ALT mechanism and showed that the FDA-approved drug ponatinib inhibits this pathway and holds exceptional promise in stopping the growth of ALT cancer cells. Our findings may provide a new direction for the treatment of ALT cancers by repurposing an FDA-approved drug for these types of tumours.”
Commenting as an independent expert, Assistant Professor Valerie Yang, medical oncologist with the Department of Lymphoma and Sarcoma at the National Cancer Centre Singapore, said: “Sarcomas and glioblastomas are both highly complex cancers that are more prevalent in young people and currently have limited treatment options. The identification of a drug that is FDA-approved which can be repurposed to target ALT, an Achilles heel in these cancers, is very exciting.”
To date, there is no clinically approved targeted treatment for ALT cancers. Furthermore, many ALT cancers, such as osteosarcoma and glioblastoma, show resistance to chemotherapy, highlighting the need for a more targeted form of treatment.
Drug affects telomeres in ALT cancer cells
Through high-throughput drug screening and subsequent testing of shortlisted compounds, the scientists discovered that ponatinib, a drug approved by the FDA for a type of bone marrow cancer, can kill ALT cancer cells effectively.
When osteosarcoma and liposarcoma cells were treated with ponatinib, the scientists found that the drug led to DNA damage, dysfunctional telomeres, and triggered senescence. Importantly, the synthesis of telomeres in the cells also dropped after 18 to 20 hours of treatment with the drug.
Pre-clinical studies conducted on mice that had received transplants of human bone cancer cells further validated the potential of ponatinib. The drug reduced the tumour sizes without affecting the mice’s body weight, a common side effect associated with cancer treatments.
In mice with tumours treated with ponatinib, there was also a reduction in a biomarker for ALT cancer as compared to untreated mice – an indicator that the drug was effective in inhibiting ALT cancer growth.
The scientists ran further tests to identify ponatinib’s mode of action on telomeres in ALT cancer cells and identified a signalling pathway (a series of chemical reactions in which a group of molecules in a cell work together to control a cell function) that could be responsible for the drug’s effect on ALT.
The researchers are now studying further how ponatinib affects telomeres to understand in more detail the signalling pathway they have identified. They are also assessing potential ponatinib-based combinatorial drug treatments for ALT cancers.
Source: Nanyang Technological University