WHO Predicts Shortfall in Syringe Production
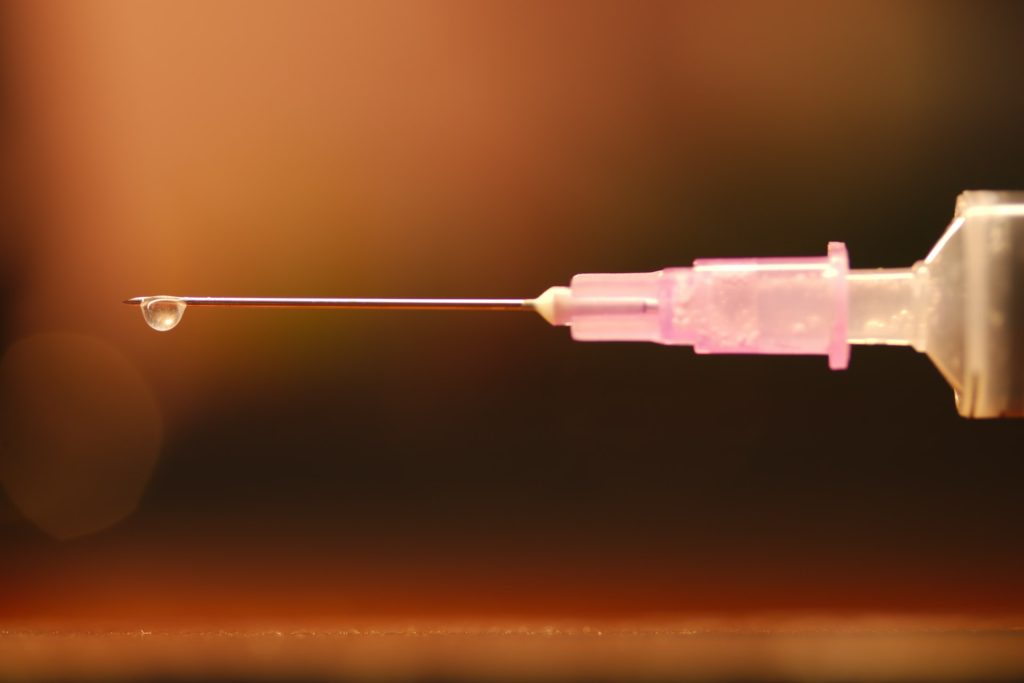
The World Health Organization has said that with the goal of two COVID vaccine doses for seven billion people between now and 2023, a shortage of at least one billion syringes “could occur”, if manufacturing does not increase. This could endanger other immunisation programmes.
Lisa Hedman, WHO Senior Advisor, from the Access to Medicines and Health Products division, warned that there could be a generation of children who miss scheduled immunisation jabs unless manufacturers come up with a way to make more single-use disposable syringes.
“When you think about the magnitude of the number of injections being given to respond to the pandemic, this is not a place where we can afford shortcuts, shortages or anything short of full safety for patients and healthcare staff,” said the WHO expert.
She told media that more than 6.8 billion doses of COVID vaccines are being administered globally per year – nearly twice the yearly number for routine inoculations.
“A shortage of syringes is unfortunately a real possibility and here’s some more numbers. That [given] the global manufacturing capacity of around six billion a year for immunisation syringes it’s pretty clear that a deficit in 2022 of over a billion could happen if we continue with business as usual.”
Reuse of syringes was inadvisable, also noting that syringes were particularly prone to transport delays because they took up 10 times the space of a vaccine.
Meanwhile, the heads of the International Monetary Fund (IMF), World Bank Group, WHO and the World Trade Organization (WTO) held a follow up session of High-Level Consultations with the CEOs of leading COVID vaccine manufacturing companies on Tuesday.
All participants at the meeting agreed on the urgency of increased vaccine dose delivery to low-income countries, where less than 2.5% of the population has been fully vaccinated.
The meeting’s aim was to identify how to ensure more equitable distribution of vaccines and all participants pledged to continue working together to clarify donations, vaccine swaps and delivery schedules, so that distribution of the life-saving vaccines can be more effectively targeted towards needy countries.
The meeting of the Multilateral Leaders Task Force on COVID-19 built on technical work undertaken by multidisciplinary teams during the months of September and October.
During the consultations, the leaders of the four organisations and the CEOs also examined how best to tackle trade-related bottlenecks; how to improve the donation process; what additional steps are needed to reach the vaccination target of 40% of people in all countries by the end of the year; and how to improve transparency and data sharing with the IMF-WHO Vaccine Supply Forecast Dashboard and the Multilateral Leaders Task Force.
The effort will require close collaboration between manufacturers, governments and the international COVAX initiative, on enhanced delivery schedules, especially for doses that are being donated.
Source: UN News






