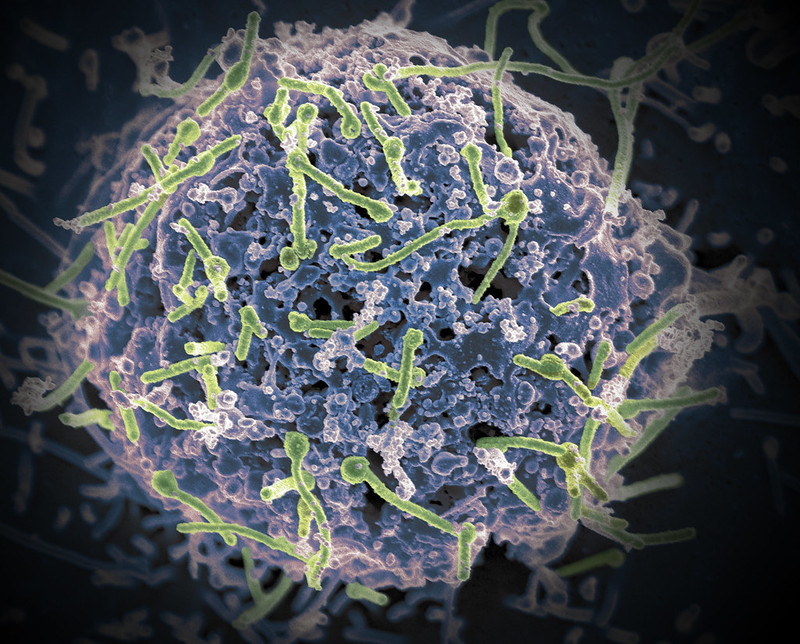
Micronutrients Could Replenish Mitochondria in Cardiac Cells

There is convincing evidence that micronutrients, such as iron, selenium, zinc, copper, and coenzyme Q10, can impact the function of cardiac cells’ energy-producing mitochondria to contribute to heart failure according to a review published in the Journal of Internal Medicine.
Research has established a relationship between poor cardiac performance and metabolic perturbations, including deficits in substrate uptake and utilisation, reduction in mitochondrial oxidative phosphorylation and excessive reactive oxygen species production. Together, these disturbances result in depletion of cardiac adenosine triphosphate (ATP) and loss of cardiac energy. Delivering more energy substrates such as fatty acids to the mitochondria will be worthless if the mitochondria can’t turn them into fuel.
Micronutrients are required to efficiently convert macronutrients to ATP. However, studies have shown that up to 50% of patients with heart failure have deficiencies in one or more micronutrients. “Micronutrient deficiency has a high impact on mitochondrial energy production and should be considered an additional factor in the heart failure equation,” the authors argued. Their findings suggest that micronutrient supplementation could represent an effective treatment for heart failure.
“Micronutrient deficiency has a high impact on mitochondrial energy production and should be considered an additional factor in the heart failure equation, moving our view of the failing heart away from ‘an engine out of fuel’ to ‘a defective engine on a path to self-destruction’,” said co–lead author Nils Bomer, PhD, of the University Medical Center Groningen, in The Netherlands.
An accompanying editorial suggests a large trial to see if there is indeed a clinical benefit.
Source: Wiley