Limpopo Measles Outbreak Continues amid Low Vaccination Rates
Since 11 October 2022, the National Institute for Communicable Diseases (NICD) seven measles cases have been detected in Greater Sekhukhune District in Limpopo province within 30 days, as of 21 October.
Infected individuals ranged from 9 months to 24 years. One child was fully vaccinated for measles, with two measles doses given in 2019. One child was unvaccinated, and the other five measles cases had unknown vaccination history. One measles case was hospitalised while one other had a complication that led to pneumonia.
District and provincial health officials have started a public health response. This includes enhanced surveillance for measles, contact tracing, screening for suspected cases using a case definition followed by collection of blood and throat swabs for measles diagnostic testing, and reviewing medical records to pick up missed cases. Vaccinations are underway for those exposed to suspected or confirmed cases.
The measles immunisation coverage data for the Greater Sekhukhune district showed a decrease of 87% to 64% for measles dose 1 and 86% to 60% for measles dose 2 from 2017 to 2022. This is below the 95% coverage needed to achieve herd immunity. A survey is being done to validate the vaccination data provided to the province and investigate factors that might be contributing to the measles outbreak. Community awareness and health promotion by healthcare workers is continuing in the district to inform the public about the spread of measles and interventions to prevent disease. Measles vaccination has been initiated for children under 15 years to increase the measles immunity in the community and to prevent further spread of measles.
Clinicians should continue to be on the alert for measles cases, especially in Limpopo Province, as large measles outbreaks are occurring in sub-Saharan Africa, including in neighbouring countries.
Signs and Symptoms
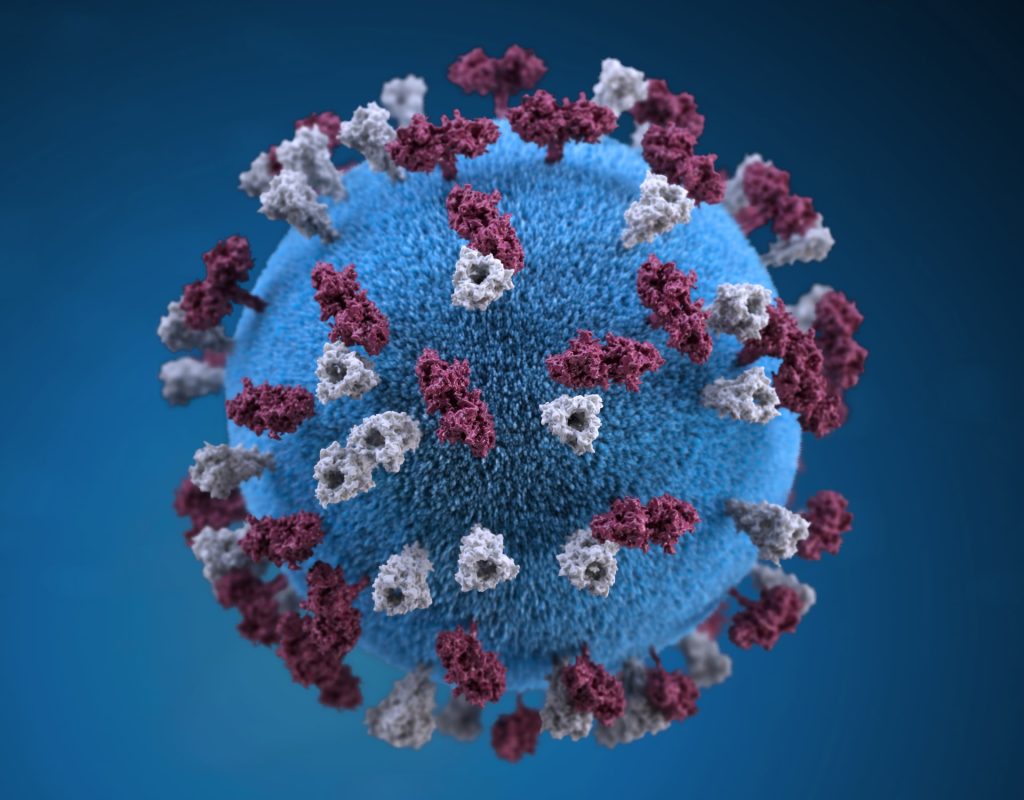
Measles is a highly contagious disease caused by a virus of the paromyxovirus family. Patients with measles present with fever and a rash. The rash looks like small, red, flat spots over the body. The rash does not form blisters, nor is it itchy or painful. Other signs include cough, conjunctivitis and coryza. Complications of measles can include diarrhoea, dehydration, encephalitis, blindness and death. Other measles complications are pneumonia, scarring of the cornea (kerato-conjunctivitis), and rarely encephalitis. Complications are more serious in very young children (under 2 years) or who are malnourished.
Clinicians and caregivers should check children’s road-to-health booklets to ensure measles vaccinations are up to date. Suspected measles cases should be notified on the NMC system. Click here to access the Case Notification form
Source: NICD








