Protect against Pertussis Cases in Vulnerable Populations with Tdap Vaccination

Post-COVID-19, there has been a notable increase in vaccine fatigue and apathy, influenced significantly by social media.1 Higher trust in social media correlates with increased vaccine hesitancy, driven by the widespread dissemination of vaccine misinformation and conspiracy theories on these platforms.1 This has significantly impacted public perceptions and trust regarding vaccinations.1
Recently, statistics have indicated a notable increase in pertussis cases in South Africa. In December 2022, the National Institute for Communicable Diseases (NICD) reported a total of 408 cases countrywide.2 Most of these cases occurred in children younger than five years old as parents might not return to their healthcare professional to have their children vaccinated after six weeks of age.2
Pertussis is a vaccine-preventable disease
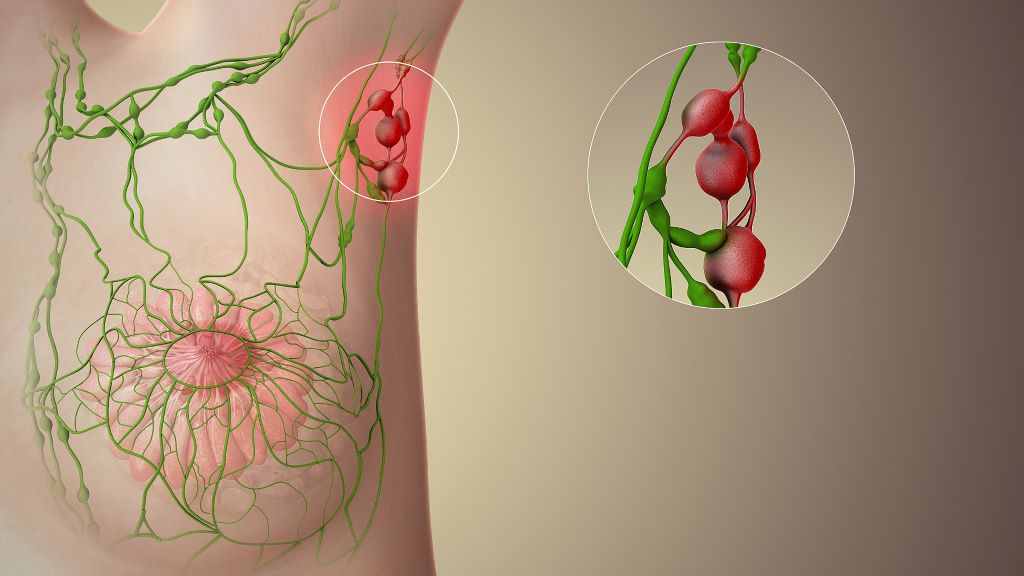
Recent research concluded that immunisation with the pertussis vaccine during pregnancy prevented 65% of pertussis infections through 6 months of age.3 These results indicate that maternal pertussis vaccination protects infants from infection during a period of greatest vulnerability to severe morbidity and mortality.3 The findings support the infant health benefits of recommendations to administer a dose of pertussis vaccine near 28 weeks of gestational age.3
Health authorities in South Africa have emphasised the importance of vaccination to control pertussis outbreaks.4 Immunity following vaccination lasts for approximately 5-6 years, necessitating booster doses.4 Episodic increases in pertussis cases occur in vaccinated populations every 3-5 years, making the completion of childhood primary series Tdap (tetanus, diphtheria, and acellular pertussis) vaccine and boosters important for prevention.4 The NICD also recommends vaccination of healthcare workers and pregnant women to reduce transmission to neonates and other vulnerable populations.4
“2024 marks the 50th anniversary of the Expanded Programme on Immunisation (EPI),” says Dr Lourens Terblanche, Vaccines Medical Head at global pharmaceutical company, Sanofi South Africa. “Every country has a national immunisation programme, and vaccines are universally recognised as best practice in terms of efficacy, tolerability, cost impact and successful public health interventions to prevent fatalities and enhance the quality of life. As we celebrate the lifesaving impact of EPI, we also need to strengthen routine immunisation initiatives, especially for pregnant women.”
Effective protection for children with Tdap vaccination
South Africa’s national immunisation schedule provides vaccinations against various diseases free of charge at state clinics, starting from birth, followed by additional doses at set times during a child’s early years.
“It is crucial to prioritise the health and well-being of patients, especially during critical stages such as pregnancy and childhood,” says Terblanche. “We urge all healthcare professionals to encourage pregnant women to receive their vaccinations timeously, and to ensure that their children’s vaccinations are up to date. Proactive efforts can significantly reduce the risk of vaccine-preventable diseases for mothers and children, safeguarding their health and the health of our communities.”
Terblanche reiterates that pertussis has the potential to cause serious and sometimes deadly complications in the paediatric population. “The majority of cases of pertussis occur in infants less than 2-3 months old, and the highest number of deaths are also seen in this age group. The situation is complicated by the fact that vaccinating infants themselves against pertussis can only start from 6 weeks of age, which is why strategies to protect them in this window of vulnerability is so important.”
Sanofi, in partnership with the National Department of Health, is urging healthcare providers throughout South Africa to encourage pregnant women to have the Tdap vaccination. Tdap vaccine Adacel is an integral component of preventive healthcare and is approved for use in individuals aged 10 through 64. This vaccine provides protection against pertussis, tetanus and diphtheria.5
Immunological response and efficacy
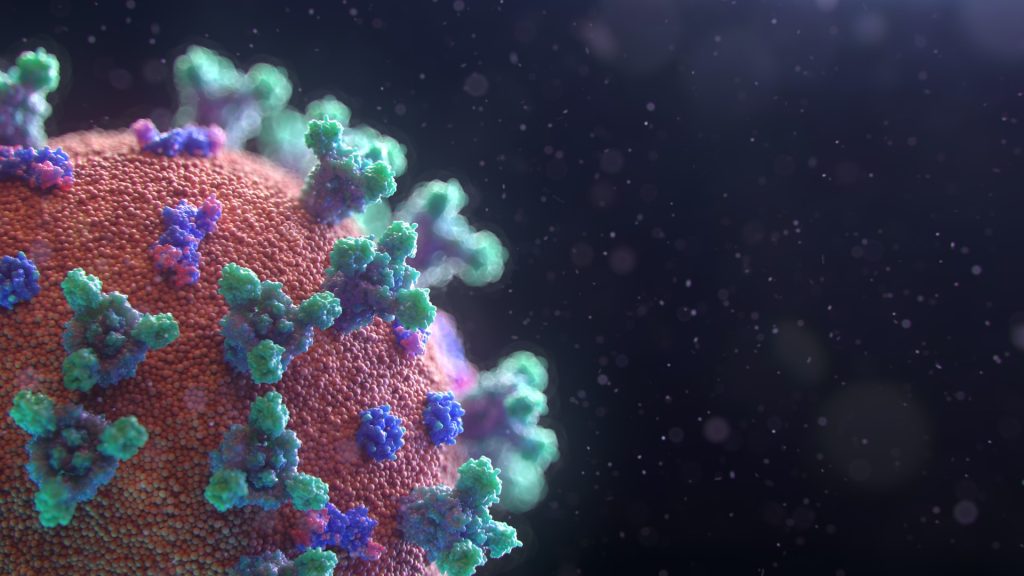
Adacel stimulates the immune system to produce antibodies that are specific to the toxins produced by tetanus and diphtheria bacteria, as well as the cells of the Bordetella pertussis bacteria. “This action provides a critical defensive shield against these diseases, with immunity that is significantly more robust and longer-lasting than natural immunity,” says Terblanche.
- Adacel is indicated for immunisation during the third trimester of pregnancy to prevent pertussis in infants younger than 2 months of age.5
- The first dose of Adacel is administered at least 5 years after the last dose of DTaP or Td.5
- Adacel is approved for a repeat vaccination as soon as 8 years after the initial Tdap dose.5
- Adacel for tetanus-prone wound management may be administered as early as 5 years after a previous dose of a tetanus toxoid-containing vaccine.5
“Adacel can help a pregnant woman to create antibodies against the bacteria that cause pertussis, and these are passed to her baby before birth,” says Terblanche.
Impact of vaccination on global health
Today, vaccines have an excellent safety record and most “vaccine scares” have been shown to be false alarms.6 However, misguided safety concerns in some countries have led to a fall in vaccination coverage, causing the re-emergence of pertussis and measles.6
Vaccinations significantly reduce disease, disability, death, and health inequities globally:6
- Public Health Impact: Vaccination has substantially lowered the incidence of diseases that were once prevalent and often fatal, contributing greatly to global health improvements comparable only to the provision of clean water.6
- Economic Benefits: By reducing disease burden, vaccination cuts healthcare costs and promotes economic growth through lower morbidity and mortality rates.6
- Global Disease Control: Successful vaccination programs have led to the eradication and control of numerous infectious diseases.6
- Herd Immunity and Social Equity: Vaccination not only protects vaccinated individuals but also contributes to broader community health through herd immunity. This indirect protection is especially beneficial in low-income settings where direct vaccine coverage may not be comprehensive.6
- Empowerment and Secondary Benefits: Beyond health, vaccination empowers women by enabling better family planning and increases educational and social opportunities through improved child survival rates.6
- Reduction of Antibiotic Resistance: By preventing bacterial infections, vaccines reduce the need for antibiotics, thereby helping to slow the development of antibiotic-resistant strains.6
With Adacel, you can help make a difference in pertussis prevention. Let’s protect mothers, children and our communities and ensure everyone has the chance to lead a healthy life by getting vaccinated.
Tdap – tetanus, diphtheria, acellular pertussis
DTaP – diphtheria, tetanus, acellular pertussis
Td – tetanus, diphtheria
References
1. Carrieri V, Guthmuller S, Wübker A. Trust and COVID-19 vaccine hesitancy. Sci Rep. 2023 Jun 7;13(1):9245. doi: 10.1038/s41598-023-35974-z. PMID: 37286569; PMCID: PMC10245358.
2. Whooping Cough Cases Increase Rapidly, Officials Urge Vigilance. Health-e News. [Accessed 22 Apr 24]. Available from: https://health-e.org.za/2023/01/27/whooping-cough-cases-increase-rapidly-officials-urge-vigilance
3. Regan AK, Moore HC, Binks MJ, et al. Maternal Pertussis Vaccination, Infant Immunization, and Risk of Pertussis. Pediatrics. 2023;152(5):e2023062664.
4. Pertussis Preparedness: An update for Physicians, Accident & Emergency practitioners and Laboratorians. National Institute for Communicable Diseases. Centre for Respiratory Diseases And Meningitis. Revised December 2022. [Accessed 22 Apr 24]. Available from: https://www.nicd.ac.za/wp-content/uploads/2022/12/Pertussis-preparedness-and-alert-doc_12-Dec-2022_Final.pdf
5. Pertussis prevention starts here. Sanofi. [Accessed 22 Apr 24]. Available from: https://www.adacelvaccine.com/
6. Andre FE, Booy R, Bock HL, et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull World Health Organ. 2008 Feb; 86(2): 140–146. Published online 2007 Nov 27. doi: 10.2471/BLT.07.040089.