New TB Drug Shows Promise, but Experimental Vaccine Disappoints

While three new tuberculosis (TB) medicines have been registered in South Africa over the last decade, TB treatment still comes with several side effects and requires taking multiple different medicines, typically for six or more months. The search for better TB medicines got a boost last week with the presentation of promising findings from a study conducted in South Africa on an experimental drug called quabodepistat. Elri Voigt reports on this and other TB studies presented at a conference in Denver, Colorado.
Arguably, the biggest TB news at the Conference on Retroviruses and Opportunistic Infections (CROI) this year was that the experimental new TB drug quabodepistat performed well in a phase 2b/c clinical trial. This means the drug can now proceed to a pivotal phase 3 trial (medicines are typically approved by regulators only after positive results in phase 3 trials).
The interim study results presented at CROI indicated that quabodepistat in combination with bedaquiline and delamanid and given for four months to people with drug susceptible TB is safe and efficacious, when compared to the six-month standard of care regimen. The standard of care regimen, currently used in South Africa’s public sector, consists of the drugs rifampicin, isoniazid, ethambutol, and pyrazinamide.
Participants were split into four study arms to either receive 10mg, 30mg or 90mg of quabodepistat (along with delamanid and bedaquline) once a day for four months or the standard of care regimen for six months. In the quabodepistat arms, a total of 98 study participants completed treatment, compared to 19 in the standard of care arm.
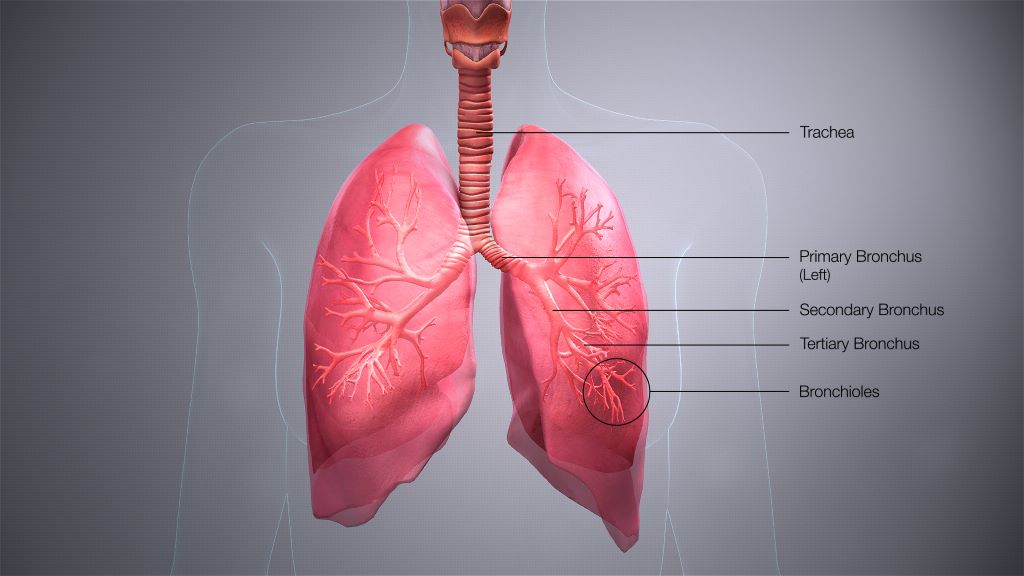
Taken together, 96% of participants in the quabodepistat arms had sputum culture conversion compared to 91% in the standard of care arm. Sputum culture conversion means TB was no longer detected in sputum samples that people coughed up when those samples were grown in the lab.
The study was conducted at several sites in South Africa and was funded by the Japanese pharmaceutical company Otsuka.
‘Furthest along’
Lindsay McKenna, the TB Project Co-Director at Treatment Action Group (TAG – a New York-based NGO), explained to Spotlight that quabodepistat is a new drug with a new mechanism of action for inhibiting TB’s cell wall synthesis. Essentially, this means that the drug interferes with the TB bacteria’s cell wall structure.
While there are a few new drugs that work the same way, quabodepistat is the furthest along.
“It’s the first in a new class of TB drugs to reach this stage since bedaquiline and delamanid were in phase 2b over ten years ago,” McKenna said.
There is however still some way to go before we will know if quabodepistat is bound for wider use than just in clinical trials. “We need to see data on clinical outcomes first,” McKenna told Spotlight, adding that quabodepistat is also being assessed in another ongoing phase 2b/c clinical trial.
“Remember that we have only seen sputum culture conversion results. Follow up is ongoing and so we will learn more when we see the proportion of participants with favorable outcomes (for example relapse free cure) 12 months post randomisation,” she said. “In the meantime, I think Otsuka should immediately begin working to start up a pre-approval access programme to enable people with unmet needs to access quabodepistat.”
Safety signals
Dr Simbarashe Takuva, Associate Director of Clinical Development at Otsuka Novel Products GmbH (an affiliate of Otsuka), who presented the results on behalf of the study team, said that overall, the quabodepistat regimen was well tolerated and considered safe.
In terms of side effects, the adverse events reported were generally described as mild or moderate, but there were some concerning signals. Grade 3 adverse events stood at 15% in the quabodepistat 10mg arm, 12% in the 30mg arm, 11% in the 90mg arm and 5% in the standard of care arm. Grade 3 adverse events are typically serious enough to prevent someone from working.
Takuva said that there were no serious adverse events (which we understand to mean grade 4/life threatening adverse events) related to the study drugs. There were also no treatment discontinuations related to the drugs. There was a single death in the study, a 25-year-old man who had met all study eligibility criteria but got sicker during the study. The study drugs were halted and standard of care drugs were given instead but the participant later died in hospital.
The researchers also looked for signs that quabodepistat might adversely affect the liver and the heart, but no safety signals related to the drugs were seen in either the liver (hepatoxicity) or the heart (cardiotoxicity).
“The data presented didn’t raise concerns about any treatment related cardio- or hepatotoxicity signals, however, it was a relatively small study, and the inclusion criteria were conservative,” McKenna commented on these findings.
One snag is that the results presented at CROI did not provide a clear answer regarding which of the three quabodepistat dosages in the study is preferable. Based on the clinical data, Takuva said it is difficult to determine which dose is best to use. He did however point out that additional work is being done looking at Pharmacokinetic and Pharmacodynamic data which will hopefully help provide more information on the ideal dose.
“Follow up on this study is ongoing. We await the final results of our phase 2 trial toward the end of the year,” he told Spotlight.
No study participants with HIV
One big limitation of these results is that the study did not enroll any people living with HIV. According to Takuva, the study had a strict exclusion criterion for the CD4 count of enrolling anyone living with HIV. A person’s CD4 count is a measure of the state of one’s immune system – higher counts are better.
Initially, the CD4 count cut off for the study was set at above 500 cells/mm3, then was amended to 350 cells/mm3 and finally it was dropped to above 250 cells/mm3 but by that time it was too late to enroll anyone living with HIV.
“The interim results are encouraging. However, I was really surprised and disappointed that they weren’t able to enroll any people living with HIV in the trial,” McKenna told Spotlight.
When asked about this, Takuva told Spotlight that the protocol did include the provision to recruit people living with HIV, but it was not feasible to include any. However, people living with HIV will be considered as important to include in any phase 3 trials going forward.
“As with all studies, we need to balance patient safety and the goal of the study outcome. In this instance, despite our best efforts, recruitment of people living with HIV was not feasible, though as we consider the possibility of a phase 3 trial, people living with HIV will remain a population that we consider important to include as far as possible in the phase 3 trial,” he said.
Treating DR-TB in people living with HIV
In contrast to the lack of people with HIV in the quabodepistat study, research was also presented at CROI looking specifically at how people living with HIV did in the landmark endTB trial. Other results from endTB were previously reported and the trial is widely considered one of a hand full of key trials transforming the treatment of drug-resistant forms of TB. The researchers found that two nine-month regimens studied in endTB did particularly well in people living with HIV. Such findings are of particular importance in a country like South Africa where many people who fall ill with TB are also living with HIV. (For those interested in the details, the two regimens were bedaquiline/linezolid/moxifloxacin/pyrazinamide and bedaquiline/clofazimine/linezolid/levofloxacin/pyrazinamide)
Some disappointments

In a disappointing development, researchers presenting at CROI reported that a study testing a three-month regimen for the treatment of drug-susceptible TB was stopped early after an interim review found the regimen had poor efficacy compared to the six-month standard of care. The regimen contained the drugs clofazimine and rifapentine, among others. It means that for now the shortest regimen for treating drug-susceptible TB validated in a clinical trial remains a four-month regimen containing the medicines rifapentine and moxifloxacin, among others. That four-month regimen is not yet in wide use, even though findings confirming its safety and efficacy were reported in 2020.
We also received some bad news on an experimental TB vaccine called H56:IC31. The idea of H56:IC31 was to vaccinate people who were just cured of TB to prevent the TB from coming back – people whose TB is deemed to be cured are known to have an increased risk of falling ill with TB again. Despite promising signs in earlier studies, the vaccine failed to reduce TB recurrence in a phase 2 clinical trial of over 800 people. Much of this study was conducted at sites in South Africa.
TB treatment’s impact on mental and physical health
Another interesting study conducted in South Africa and presented at CROI looked at the changes in mental and physical health that people ill with TB experience before and after treatment. It found that the quality of life and physical fitness of participants was reduced at the start of TB treatment but did improve by the end of TB treatment.
The researchers looked at 200 study participants split between South Africa, Zambia, Malawi, Mozambique and Zimbabwe. Their mental and physical health was assessed when they started TB treatment through a standardised short form quality of life survey, depression assessed through a patient health questionnaire and their physical health was tested using a six-minute walk test. Participants were assessed again when treatment was completed, and data was compared to see what changed between the start and end of TB treatment.
Overall, participant’s physical quality of life increased by 39% by the end of TB treatment, mental quality of life increased by 19%, ability to do a six-minute walk increased by 15% and depression scores decreased by 26%.
Long-acting therapies for TB
Long-acting therapies have been making waves for some time in HIV treatment and a long-acting injection and ring are currently being offered in pilot projects in South Africa. Two studies of long-acting therapies in mice presented at CROI show that there is at least some movement in this area as well when it comes to TB. Such long-acting therapies have particular potential for TB preventive therapy – with for example what is now a three-month course of pills being administered as a single long-acting injection.
One study found that a long-acting injectable form of the drug rifapentine had similar efficacy to a one-month course of preventive therapy in pill form, while another had similarly promising findings for an injection using a long-acting formulation of a diarylquinoline (a class of TB drugs that include bedaquiline). It is anticipated these early proof of concept mouse studies will be followed by studies in humans.
Republished from Spotlight under a Creative Commons licence.
Source: Spotlight