Researcher Discovers Ancient Egyptian Mugs Contained Hallucinogens
The first-ever physical evidence of hallucinogens in an Egyptian mug has been found, validating written records and centuries-old myths of ancient Egyptian rituals and practices. Through advanced chemical analyses, University of South Florida professor Davide Tanasi examined one of the world’s few remaining Egyptian Bes mugs.
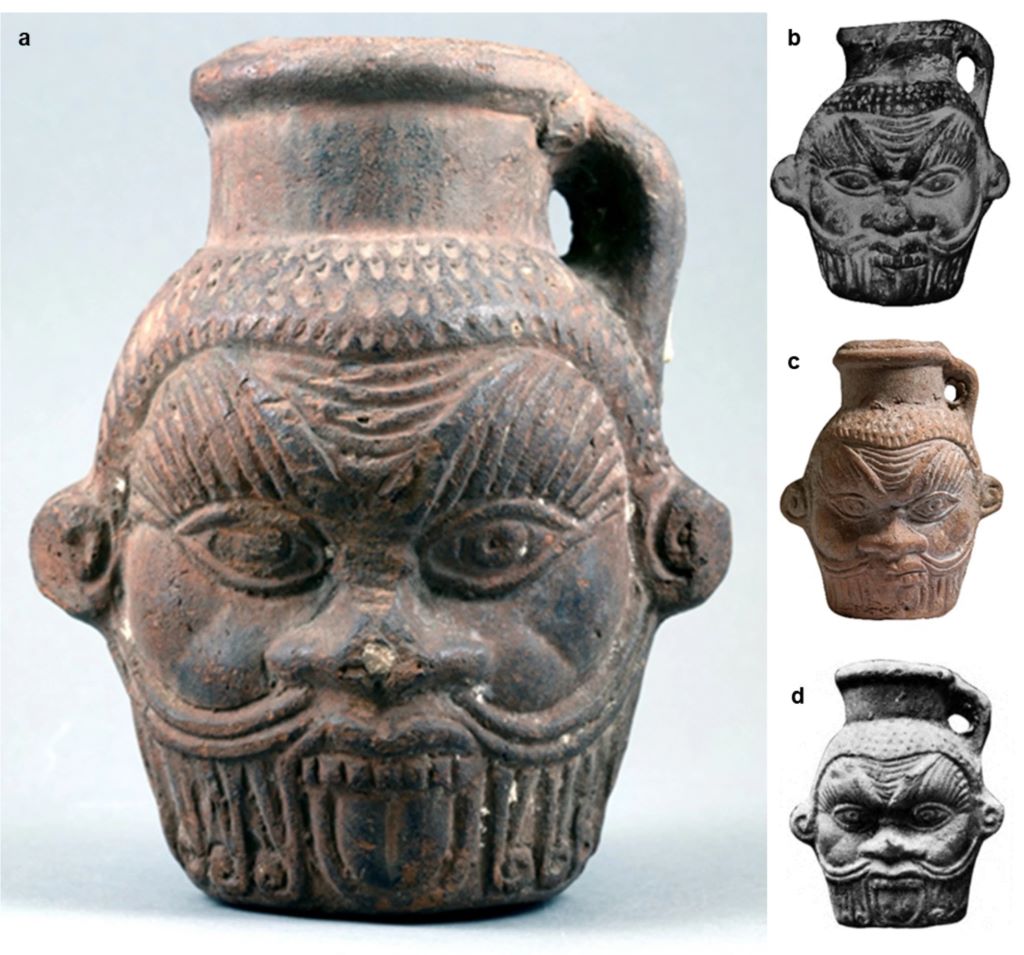
Such mugs, including the one donated to the Tampa Museum of Art in 1984, are decorated with the head of Bes, an ancient Egyptian god or guardian demon worshiped for protection, fertility, medicinal healing and magical purification. Published in Nature’s Scientific Reports, the study sheds light on an ancient Egyptian mystery: The secret of how Bes mugs were used about 2000 years ago.
“There’s no research out there that has ever found what we found in this study,” Tanasi said. “For the first time, we were able to identify all the chemical signatures of the components of the liquid concoction contained in the Tampa Museum of Art’s Bes mug, including the plants used by Egyptians, all of which have psychotropic and medicinal properties.”
The presence of Bes mugs in different contexts over a long period of time made it extremely difficult to speculate on their contents or roles in ancient Egyptian culture.
“For a very long time now, Egyptologists have been speculating what mugs with the head of Bes could have been used for, and for what kind of beverage, like sacred water, milk, wine or beer,” said Branko van Oppen, curator of Greek and Roman art at the Tampa Museum of Art. “Experts did not know if these mugs were used in daily life, for religious purposes or in magic rituals.”
Several theories about the mugs and vases were formulated on myths, but few of them were ever tested to reveal their exact ingredients until the truth was extracted layer by layer.
Tanasi, who developed this study as part of the Mediterranean Diet Archaeology project promoted by the USF Institute for the Advanced Study of Culture and the Environment, collaborated with several USF researchers and partners in Italy at the University of Trieste and the University of Milan to perform chemical and DNA analyses. With a pulverised sample from scraping the inner walls of the vase, the team combined numerous analytical techniques for the first time to uncover what the mug last held.
The new tactic was successful and revealed the vase had a cocktail of psychedelic drugs, bodily fluids and alcohol – a combination that Tanasi believes was used in a magical ritual re-enacting an Egyptian myth, likely for fertility. The concoction was flavoured with honey, sesame seeds, pine nuts, liquorice and grapes, which were commonly used to make the beverage look like blood.
“This research teaches us about magic rituals in the Greco-Roman period in Egypt,” Van Oppen said. “Egyptologists believe that people visited the so-called Bes Chambers at Saqqara when they wished to confirm a successful pregnancy because pregnancies in the ancient world were fraught with dangers. So, this combination of ingredients may have been used in a dream-vision inducing magic ritual within the context of this dangerous period of childbirth.”
“Religion is one of the most fascinating and puzzling aspects of ancient civilizations,” Tanasi said. “With this study, we’ve found scientific proof that the Egyptian myths have some kind of truth and it helps us shed light on the poorly understood rituals that were likely carried out in the Bes Chambers in Saqqara, near the Great Pyramids at Giza.”
The Bes mug is on display now at the Tampa Museum of Art and can be viewed in the exhibition, “Prelude: An Introduction to the Permanent Collection.” View a 3D model of the Bes mug produced by the USF Institute for Digital Exploration.