An End to The ‘Therapeutic Drought’ in Atopic Dermatitis

The end of a longstanding “therapeutic drought” in atopic dermatitis (AD) is in sight as improved understanding of the pathogenesis and pathophysiology has stoked development of multiple drug candidates, according to a leading expert in the field.
“We did have treatments like cyclosporine, that are not specific as we know, and they are not treatments we can give our patients for long-term disease control,” said Emma Guttman-Yassky, MD, of the Icahn School of Medicine at Mount Sinai, during the Inflammatory Skin Diseases Summit.
She said that overcoming this drought was not easy, mostly because “we didn’t have enough understanding of the disease and its pathogenesis, really preventing therapeutic development for patients with atopic dermatitis,” she said.
New AD therapies built on the trail made for psoriasis treatment, starting with basic studies that produced insights into pathogenesis, leading to hypotheses that eventually could be tested in clinical trials, she said. Progress was accompanied by many failures in early stages of therapeutic development in psoriasis.
“One failure that I remember very vividly from psoriasis was the failure of interferon-gamma targeting,” Dr Guttman-Yassky recounted. “In atopic dermatitis, we also had our share of this type of failure, but these failures really helped shape therapeutic directions for all the diseases we are now targeting, including atopic dermatitis.”
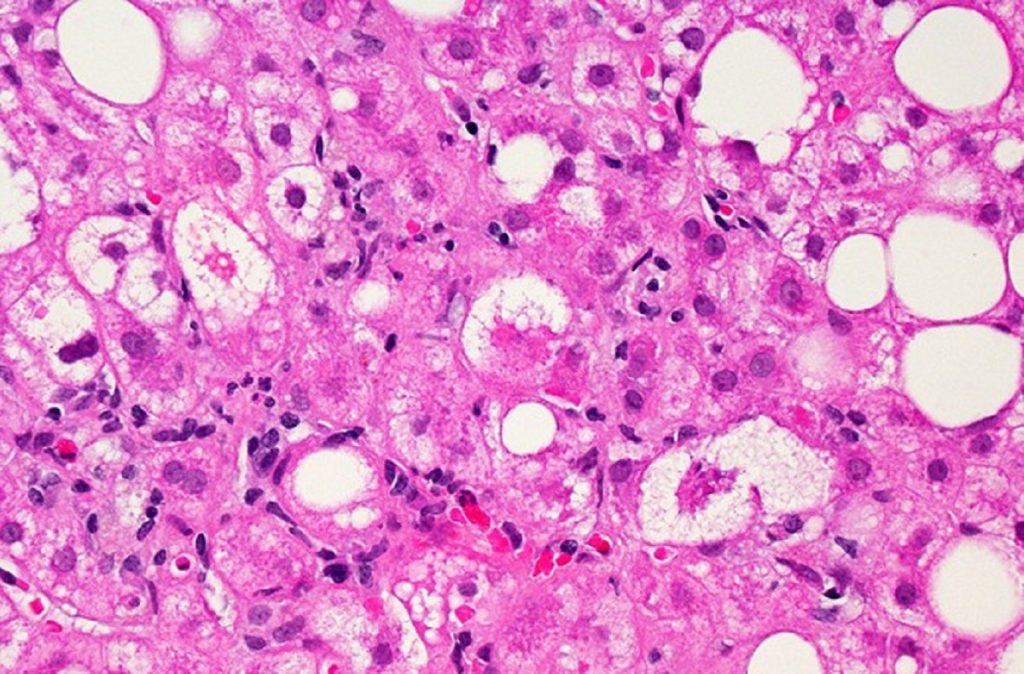
This rocky development has led to recognition that AD is a complex disease involving multiple pathogenetic components, including barrier dysfunction, immune abnormalities, disruption of the dermal microbiome, and the peripheral and central nervous systems that play a central role in itch and other disease manifestations.
“Of all the major components involved in AD pathogenesis, immune targeting is the most tractable,” said Dr Guttman-Yassky. “Immune abnormalities are the most important because they perpetuate the disease phenotype of atopic dermatitis, from the nonlesional skin to acute disease and chronic lesions.”
In contrast to psoriasis, AD is a more heterogeneous disease with multiple clinical phenotypes that correlate with differences in immune polarisation and barrier dysfunction. All of the phenotypes exhibit activation of the type 2 inflammatory pathway as a common feature. Across the spectrum of clinical phenotypes, additional cytokine targeting may be required to achieve disease control.
Understanding that AD arises from systemic inflammation has also helped therapy development. Several studies have suggested that, compared to psoriasis, AD is associated with higher levels of immune activation. Blood samples of patients with AD have shown increased levels of activated T cells, circulatory cytokines, and cardiovascular markers.
The accumulation of new insights into AD pathogenesis added no fewer than a dozen viable therapeutic candidates to the pipeline. Dupilumab (Dupixent) led the way in providing the proof of principle that Th2-specific targeting reverses key pathogenetic factors that drive the disease process in AD.
Dr Guttman-Yassky pointed out how targeting Th2 inflammation with dupilumab led to reversal of barrier defects and lichenisation typical of AD as early as 4 weeks, and that by 16 weeks lesional and nonlesional skin looked similar. Furthermore, markers of epidermal hyperplasia and proliferation were “completely wiped out.”
Dr Guttman-Yassky highlighted several key classes of AD drug candidates with potential to build on the success of targeting inflammation: Interleukin-13 inhibition, OX40 inhibition and JAK/STAT inhibition, which showed promising results.
“With these types of response rates, our treatment goals for our patients are evolving,” said Dr Guttman-Yassky.
Source: MedPage Today