Searching for Broad-spectrum Antiviral Agents for the Next Pandemic

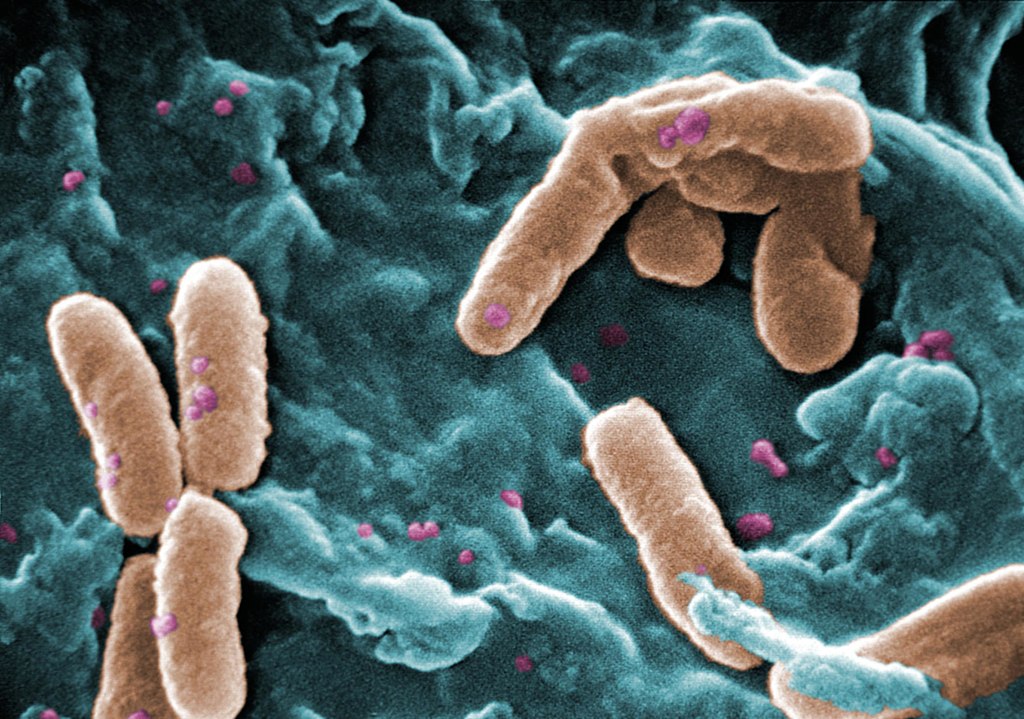
A new study has identified potential broad-spectrum antiviral agents that can target multiple families of RNA viruses with pandemic potential. The study, published in Cell Reports Medicine, tested an array of innate immune agonists that work by targeting pathogen recognition receptors, and found several agents that showed promise, including one that exhibited potent antiviral activity against members of RNA viral families.
The authors say recent epidemics as well as global climate change and the continuously evolving nature of the RNA genome indicate that arboviruses, viruses spread by arthropods such as mosquitoes, are prime candidates for the next pandemic after COVID. These include Chikungunya virus (CHIKV), Dengue virus, West Nile virus and Zika virus. The researchers write: “Given their already-demonstrated epidemic potential, finding effective broad-spectrum treatments against these viruses is of the utmost importance as they become potential agents for pandemics.”
Led by Gustavo Garcia Jr. in the UCLA Department of Molecular and Medical Pharmacology, researchers found that several antivirals inhibited these arboviruses to varying degrees. “The most potent and broad-spectrum antiviral agents identified in the study were cyclic dinucleotide (CDN) STING agonists, which also hold promise in triggering an immune defence against cancer,” said senior author Vaithi Arumugaswami, Associate Professor in the UCLA Department of Molecular and Medical Pharmacology.
“A robust host antiviral response induced by a single dose treatment of STING agonist cAIMP is effective in preventing and mitigating the debilitating viral arthritis caused by Chikungunya virus in a mouse model. This is a very promising treatment modality as Chikungunya virus-affected individuals suffer from viral arthritis years and decades from the initial infection,” Arumugaswami added.
“At molecular level, CHIKV contributes to robust transcriptional (and chemical) imbalances in infected skin cells (fibroblasts) compared to West Nile Virus and ZIKA Virus, reflecting a possible difference in the viral-mediated injury (disease pathogenesis) mechanisms by viruses belonging to different families despite all being mosquito-borne viruses,” said senior author Arunachalam Ramaiah, Senior Scientist in the City of Milwaukee Health Department.
“The study of transcriptional changes in host cells reveals that cAIMP treatment rescues (reverses) cells from the harmful effect of CHIKV-induced dysregulation of cell repair, immune, and metabolic pathways,” Ramaiah added.
The study concludes that the STING agonists exhibited broad-spectrum antiviral activity against both arthropod-borne- and respiratory viruses, including treaded SARS-CoV-2 and Enterovirus D68 in cell culture models.
Garcia notes, “The next step is to develop these broad-spectrum antivirals in combination with other existing antivirals and be made readily available in the event of future respiratory and arboviral disease outbreaks.”
Source: University of California – Los Angeles Health Sciences