Snake Antivenom Mired by Shortages and Side-effects – Could a New Treatment Boost Our Options?
By Jesse Copelyn

In recent years, shortages of snake antivenom have plagued South Africa and much of the globe. Even when antivenom is available, potentially serious side effects often limit its use. Jesse Copelyn unpacks the fascinating details behind the antivenom products that might save your life and takes a look at a promising experimental treatment.
Every day, somewhere between 220 and 380 people die from snakebite around the world, yet according to Doctors Without Borders (MSF) the problem remains “chronically underfunded and neglected”.
MSF’s senior advisor on neglected tropical diseases, Koert Ritmeijer, tells Spotlight that in 2019 the World Health Organization (WHO) committed to halve the number of snakebite deaths by 2030. But this hasn’t been followed by any significant support from donor countries or philanthropic foundations, he says, with programmes that aim to “increase patients’ access to antivenoms [remaining] very underfunded”.
Antivenom is the primary registered class of treatments for snakebite. Long-running global shortages of the treatment continue to leave patients in poorer parts of the world without the care they need. That’s in part because pharmaceutical companies haven’t always found it profitable to produce. The treatment takes a long time to manufacture and it has to be geared to a specific or small group of snake species. The clientele are often those that are least able to pay, namely Africa and Asia’s rural poor.
With a limited number of suppliers, and thus a lack of market competition, prices remain high, making it difficult for many African governments to import antivenom without donor assistance.
South Africa has long been an exception. It’s the only country in Sub-Saharan Africa that produces its own antivenom – which is internationally recognised and outperforms several comparable products when studied in mice. Additionally, research done in the Western Cape shows that hospital pharmacies have traditionally had stock on hand.
However, last year production delays at the country’s state-run manufacturer, the South African Vaccine Producers (SAVP), led to a nation-wide shortage of antivenom, leaving many snakebite victims with limited options. The locally made SAVP products (previously the SAIMR) have historically been the main source of antivenom in the country.
While the nation-wide stockouts were reportedly resolved within a few months, this appears to have been more than a one-time blip. Even before the national shortage made news headlines last year, neighbouring countries that rely on South African antivenom were struggling to procure enough of the product. For instance, a 2022 study states that supply to Eswatini was becoming “increasingly and disturbingly intermittent” and that a charitable foundation there had “been unable to secure a supply of this antivenom for several months”.
Meanwhile, CEO of the African Snakebite Institute, Johan Marais told Spotlight that vets in South Africa have been struggling to access sufficient supplies for the last three years (the same SAVP products that are used to treat humans are sometimes used on pet dogs that get bitten). He said stocks in the country were low heading into snakebite season – spring and summer.

Compounding the problem is that even at the best of times, people in poor rural areas often struggle to access antivenom shortly after being bitten (even though the issue can be extremely time-sensitive). That’s because patients can’t simply get the drug at a local pharmacy or out of their medicine cabinet. Instead, they need to wait until they arrive at an intensive care unit before doctors can assess whether they require the treatment – and if they do, it has to be administered intravenously under carefully monitored conditions.
This is because antivenom comes with a range of side-effects. For instance, research at a Kwazulu-Natal hospital found that over three in five patients had some adverse reaction to the antidote, with nearly half of all patients going into anaphylactic shock, a severe allergic reaction that causes a person’s blood pressure to drop and makes it difficult to breathe. Consequently, health workers need to be on standby with adrenaline.
People who get bitten in rural areas far away from large healthcare facilities are thus often left in a precarious position despite being most at risk.
But why do antivenom products have so many side-effects in the first place? And why are they so difficult and time-consuming to manufacture? The answer has to do with the archaic way that antivenom is made.
A life-saving drug made of ‘horse junk’
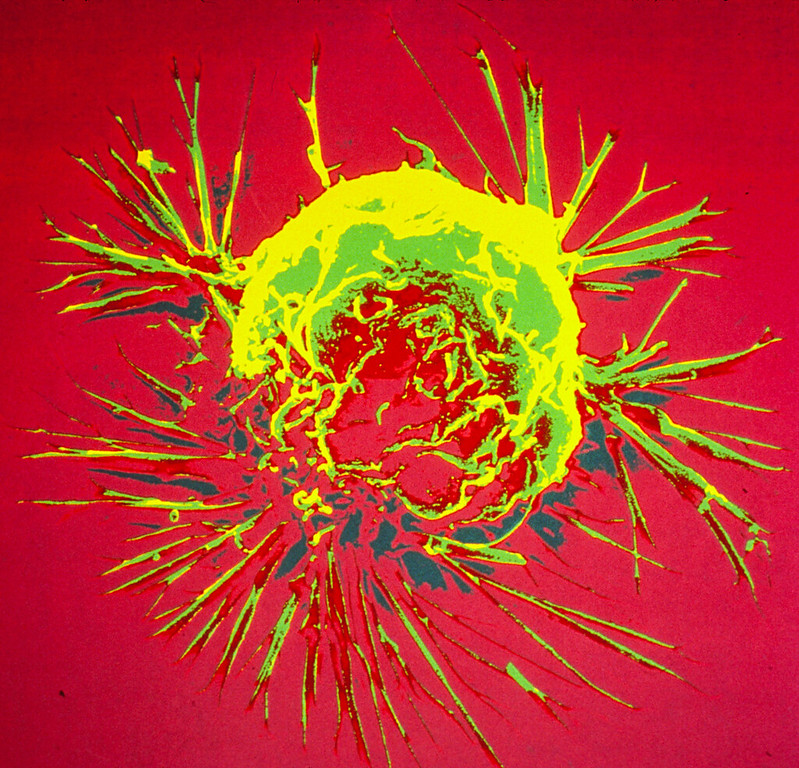
In South Africa, the SAVP, which is a subsidiary of the National Health Laboratory Services (NHLS), makes antivenom by injecting small amounts of snake venom into a horse, so that the animal’s immune system can learn to recognise and combat the toxins. This is done repeatedly over a period of nine months until the horse becomes hyperimmunised, meaning its body produces massive numbers of antibodies which target the venom.
NHLS spokesperson, Mzi Gcukumana, says that once this happens, the horse’s “plasma is collected” (this is the liquid part of blood that contains the antibodies), and is then “carefully filtered in a sterile environment”.
The result is an antivenom product which targets the snake species that was used on the horse in the first place. At present, the SAVP makes three antivenoms: one for boomslang bites, another which is used for the saw-scaled viper, and a third, which treats bites from 10 different snake species found across the country, including the puff adder and rinkhals (which are some of the most common culprits of snakebite in South Africa). This multi-species product, known as a polyvalent antivenom, is made by injecting the horse with venom from different snake species.
There’s nothing unusual about the SAVP’s method – it’s the way everyone has made commercial snake antivenoms since the late 19th century (in some countries sheep are used instead of horses) and while it’s effective, it is also well-understood why it often induces serious side-effects.
Dr Kurt Wibmer, a scientist who is researching a new snakebite treatment, explains that with antivenom “only 10 to 20 percent of the medicine you’re getting is specific to the venom, and the other 80% is junk horse protein that your body doesn’t [need].” The result is that by injecting antivenom “you’re putting a bunch of foreign substances into your body, that the body then recognises as ‘not you’, and it develops an immune response to that [which can sometimes be extreme]”.
To add to these problems, antivenom is expensive. According to price lists shared with Spotlight by staff at the Tygerberg Poison Information Centre, the SAVP’s polyvalent product is currently priced at R2 400 per vial, while the boomslang product is sold for R7 700. And since most of the vial is “junk horse protein”, snakebite victims require multiple hits to get enough of the active ingredient. This could be 6 vials or it could be over 20.
With a high price tag, a laborious production process, and a host of side-effects that prevent health workers from saving snakebite victims at primary healthcare facilities, new treatments are badly needed – either to replace traditional antivenom or to complement it. Fortunately, many are being designed to address exactly these problems.
Over a hundred years later, anti-inflammatory drug may expand treatment options
One promising treatment in development is a synthetic anti-inflammatory medicine called Varespladib. This drug was originally developed as a treatment for conditions like acute coronary syndrome. After these efforts were abandoned, scientists discovered that the product may be able to play a role in treating snakebite victims.
That’s because Varespladib works by inhibiting an enzyme called sPLA2. sPLA2 is a core component of the venom of roughly 95% of vipers and elapids (two prominent venomous snake families). In fact, the enzyme plays a key role in many of the most harmful effects of this venom, including its ability to damage body tissue, paralyse victims, and cause heavy bleeding.
It is early days. Until now, the only evidence that suggests that Varespladib can block these effects is from studies done on mice and in petri dishes. However, a phase 2 clinical trial on humans, which has yet to be published, was just completed in the United States and India. In this research, snakebite victims who arrived at hospitals were randomly split into two groups: one got the Varespladib alongside standard treatment (like antivenom), while the other group got a placebo, plus ordinary treatment.
The results from the trial are currently under peer-review, though preliminary findings have been presented at conferences. Dr Matthew R Lewin, a co-author of the study and founder of a public benefit company that is developing the drug, told Spotlight that it looked like Veraspladib may help snakebite patients if used immediately (and when used alongside traditional treatment): “In the [trial] we took patients as long as 10 hours [after they had been bitten]. Up to 5 hours, we saw promising outcomes [from those who got Varespladib]… after 5 hours, the benefit was not apparent with respect to the primary outcome of the study”.
Time will tell whether these results will be confirmed not only in the peer-review process, but also in larger clinical trials (the present study only aimed to enrol 94 participants). If successful, Varespladib could represent an important advance.
That’s because safety trials show that unlike antivenom, the synthetic drug does not appear to cause any major side-effects. It can also be taken in pill-form, rather than being injected. This means that while snakebite victims would still have to wait until they got to a hospital to take antivenom, they would at least have something which they could take right away. While the study only looked at the effects of varespladib in combination with antivenom, Lewin suggests that “it is reasonable to expect that there will be a range of salutary [health-giving] effects” from varespladib alone, since it blocks sPLA2. He notes, however, that more research is needed.
And Varespladib isn’t the only new treatment in development. Others include a chelating agent which targets a metal-based component of snake venom. Though the evidence for this is so far only from studies in mice.
Nonetheless, since our primary treatment option for snakebite remains similar to what it was over a century ago, researchers are hopeful that we might finally begin to take a few steps forward.
Note: This is part 1 of a two-part Spotlight series on snakebite treatment in South Africa. In part 2 we will, among others, look at promising advances that may help reduce antivenom shortages.
Republished from Spotlight under a Creative Commons licence.