Newer Diabetes Drugs don’t Increase Risk to Foetus

Newer diabetes medicines do not appear to increase the risk of birth defects. The largest comparative study to date found no increased risk compared to treatment with insulin, which is considered safe during pregnancy. The study was published in JAMA Internal Medicine.
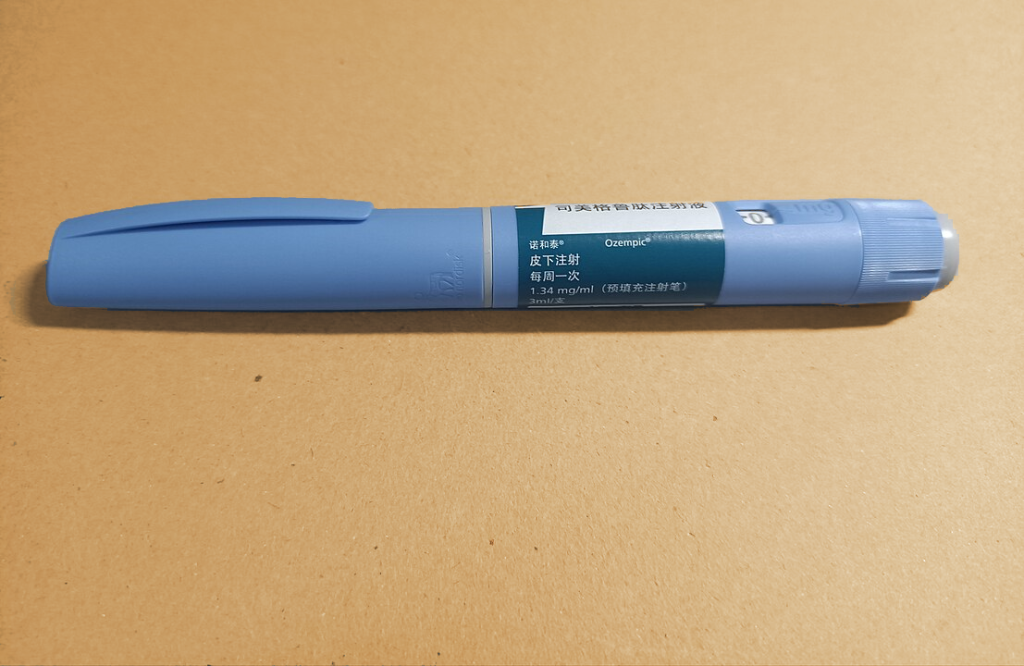
Newer diabetes drugs such as sulfonylureas, DPP-4 inhibitors, GLP-1 receptor agonists and SGLT2 inhibitors are being increasingly used, both in the treatment of diabetes, but also extended indications for several of the preparations.
However, knowledge of the foetal effects of these drugs is still low, so women with type 2 diabetes are often advised to switch to insulin before a planned pregnancy because it is considered safe. However, not all pregnancies are planned and more and more people are becoming pregnant while being treated with these drugs.
An international research team has now investigated whether the use of these drugs during pregnancy increases the risk of birth defects. The researchers used health data from 3.5 million pregnancies in six different countries (Sweden, Norway, Finland, Iceland, USA and Israel) between 2009 and 2021. Among these 3.5 million women, nearly 52 000 were diagnosed with type 2 diabetes and more than 8000 took one of the newer diabetes drugs in the three months before or after their last menstrual period.
Diabetes itself poses a risk of birth defects. High blood sugar levels in early pregnancy, which are more common in people with diabetes, increase the risk of foetal malformations. Therefore, the researchers were not surprised to see a slightly elevated risk in this group.
Among women diagnosed with type 2 diabetes before pregnancy, 5.3% of babies were born with severe birth defects, including 2.2% with heart defects, compared to the overall group where 3.8% had severe birth defects and 1.3% with heart defects.
No increased risk of birth defects
However, the researchers found that the women with diabetes treated with the newer diabetes drugs did not have a higher risk of giving birth to children with birth defects than the women with diabetes treated with insulin.
“It has already been shown that insulin is safe to use during pregnancy and that it does not cross the placenta. The increased risk of birth defects in the children of women with type 2 diabetes using the newer diabetes drugs is therefore very likely caused by the disease,” says first author Carolyn Cesta, Associate Professor at the Center for Drug Epidemiology at Karolinska Institutet.
Despite being the largest study in this field to date, covering more than 3.5 million pregnancies, relatively few women used the new diabetes drugs, and the researchers stress that further studies are needed to confirm the results. However, they note that the study still shows that these drugs do not pose a major risk of birth defects.
As type 2 diabetes becomes more common among women of childbearing age and as GLP-1 receptor agonists such as semaglutide (Wegovy, Ozempic) are approved to treat obesity, the number of exposed pregnancies is likely to increase.
“Our findings provide a first indication of the safety of infants exposed to these medications during pregnancy,” says Carolyn Cesta.
Source: Karolinska Institutet