Could Diamond Dust Replace Gadolinium in MRI?

An unexpected discovery surprised a scientist at the Max Planck Institute for Intelligent Systems in Stuttgart: nanometre-sized diamond particles, which were intended for a completely different purpose, shone brightly in a magnetic resonance imaging experiment – outshining the actual contrast agent, the heavy metal gadolinium.
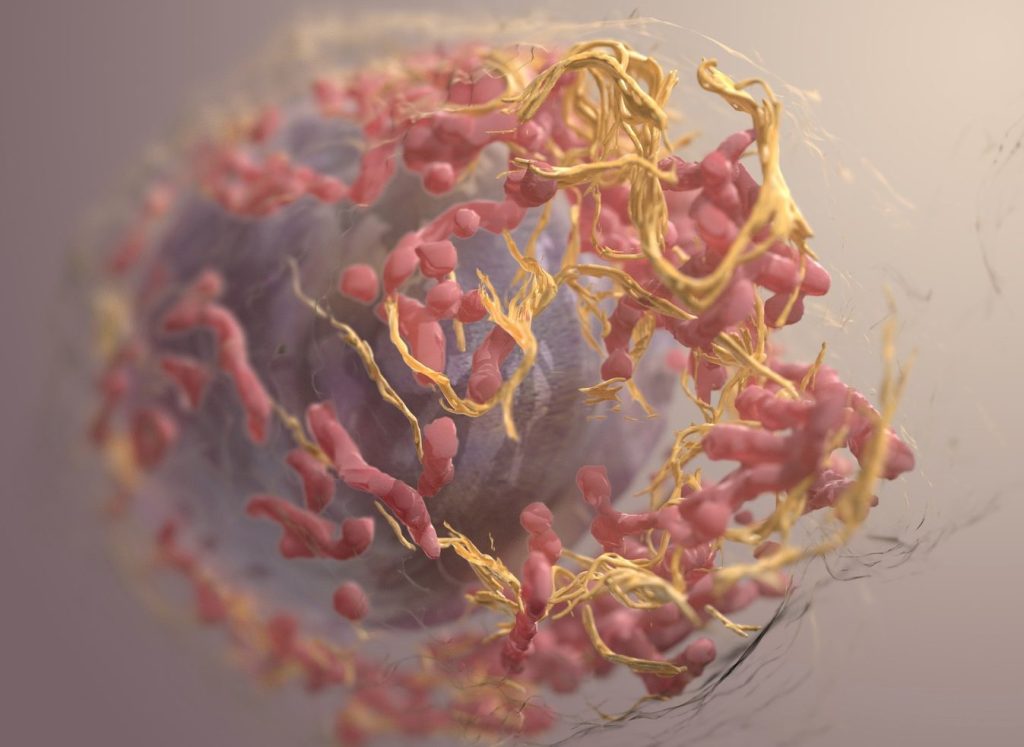
The researchers, publishing their serendipitous discovery in Advanced Materials, believe that diamond nanoparticles, in addition to their use in drug delivery to treat tumour cells, might one day become a novel MRI contrast agent.
While the discovery of diamond dust’s potential as a future MRI contrast agent may never be considered a turning point in science history, its signal-enhancing properties are nevertheless an unexpected finding which may open-up new possibilities: diamond dust glows brightly even after days of being injected.
Perhaps it could replace gadolinium, which has been used in clinics to enhance the brightness of tissues to detect tumours, inflammation, or vascular abnormalities for more than 30 years. But when injected into a patient’s bloodstream, gadolinium travels not only to tumour tissue but also to surrounding healthy tissue. It is retained in the brain and kidneys, persisting months to years after the last administration and its long-term effects are not yet known. Gadolinium also causes a number of other side effects, and the search for an alternative has been going on for years.
Serendipity often advances science
Could diamond dust, a carbon-based material, become a well-tolerable alternative because of an unexpected discovery made in a laboratory at the Max Planck Institute for Intelligent Systems in Stuttgart?
Dr Jelena Lazovic Zinnanti was working on an experiment using nanometre-sized diamond particles for an entirely different purpose. The research scientist, who heads the Central Scientific Facility Medical Systems at MPI-IS, was surprised when she put the 3–5nm particles into tiny drug-delivery capsules made of gelatin. She wanted these capsules to rupture when exposed to heat. She assumed that diamond dust, with its high heat capacity, could help.
“I had intended to use the dust only to heat up the drug carrying capsules,” Jelena recollects.
“I used gadolinium to track the dust particles’ position. I intended to learn if the capsules with diamonds inside would heat up better. While performing preliminary tests, I got frustrated, because gadolinium would leak out of the gelatin – just as it leaks out of the bloodstream into the tissue of a patient. I decided to leave gadolinium out. When I took MRI images a few days later, to my surprise, the capsules were still bright. Wow, this is interesting, I thought! The diamond dust seemed to have better signal enhancing properties than gadolinium. I hadn’t expected that.”
Jelena took these findings further by injecting the diamond dust into live chicken embryos. She discovered that while gadolinium diffuses everywhere, the diamond nanoparticles stayed in the blood vessels, didn’t leak out and later shone brightly in the MRI, just as they had done in the gelatin capsules.
While other scientists had published papers showing how they used diamond particles attached to gadolinium for magnetic resonance imaging, no one had ever shown that diamond dust itself could be a contrast agent. Two years later, Jelena became the lead author of a paper now published in Advanced Materials.
“Why the diamond dust shines bright in our MRI still remains a mystery to us,” says Jelena.
She can only assume the reason is the dust’s magnetic properties: “I think the tiny particles have carbons that are slightly paramagnetic. The particles may have a defect in their crystal lattice, making them slightly magnetic. That’s why they behave like a T1 contrast agent such as gadolinium. Additionally, we don’t know whether diamond dust could potentially be toxic, something that needs to be carefully examined in the future.”