CT Scans Improve Outcomes for Concussion Patients

A study found that CT scans for concussion patients provide crucial information on their risk for long-term impairment and their potential to make a complete recovery, and points to the need for more follow-up.
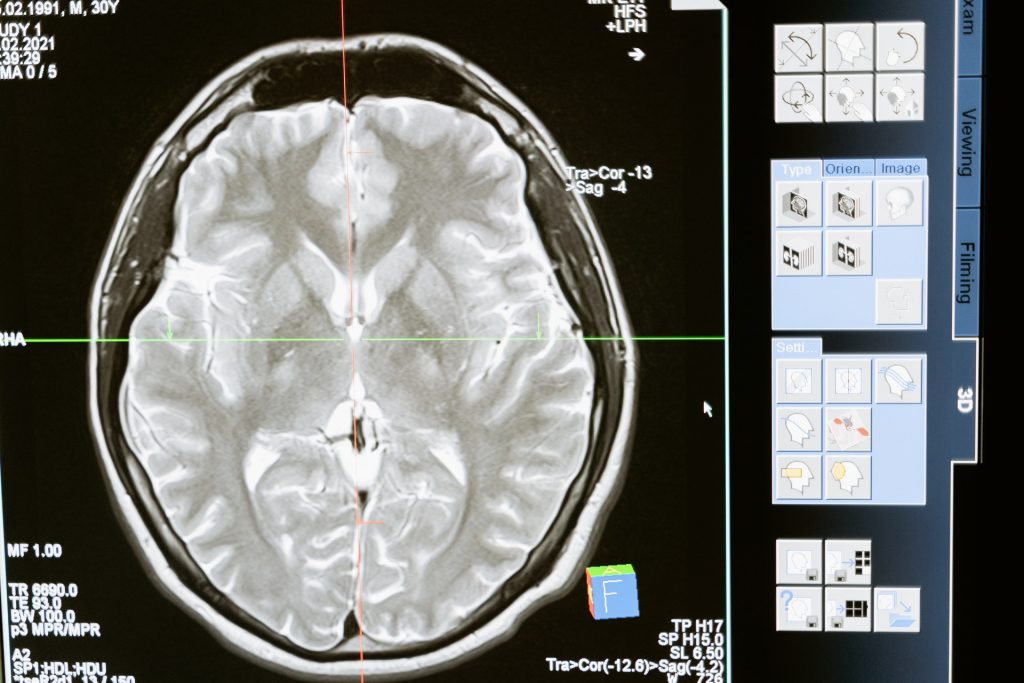
In the UC San Francisco-led study, researchers examined CT scans of 1935 patients, aged 17 and over, whose neurological exams met criteria for concussion, or mild traumatic brain injury (TBI). Outcomes for moderate and severe TBI have been linked to CT imaging features, but this may be the first time this link has been identified in patients with concussion. This contradicts previous research which had found no prognostic significance of specific types of CT abnormalities.
“Radiologists who routinely read trauma scans know intuitively that patterns of intracranial injury on CT are not random,” said first author Esther Yuh, MD, PhD, of the UCSF Department of Radiology and Biomedical Imaging. “We showed there are patterns of injury, that some of these are associated with worse outcome than others, and that they provide a window into mechanisms of injury that is reproducible across large studies.”
The study was published online in JAMA Neurology.
“Although concussions are referred to as mild traumatic brain injuries, there is nothing mild about some concussions,” explained senior author Geoffrey Manley, MD, PhD, professor and vice chair of neurological surgery at UCSF and chief of neurosurgery at Zuckerberg San Francisco General Hospital. “Patients with concussion may suffer from prolonged headache, poor sleep and impaired concentration, and they are at higher risk of self-medicating with drugs and alcohol. Concussion can also contribute to depression and anxiety, and increase the risk for suicide. We need to view concussion not as an event but as a disease requiring physician follow-up after a patient is discharged from the hospital.”
The participants were enrolled by the brain injury research initiative TRACK-TBI, of which Manley is the principal investigator. To enrich the number of so-called complicated concussions, the researchers drew exclusively from patients who had been seen at hospitals with level 1 trauma centres. This meant 37 percent of study participants had a positive CT, significantly more than the 9 percent of positive CTs from patients in US emergency departments.
The most common patterns of injury, affecting more than half of CT-positive patients, were combinations of subarachnoid haemorrhage (SAH), subdural haematoma (SDH), and/or contusion, which may be caused by injuries such as falls from standing. About 7 percent had intraventricular haemorrhage (IVH) or petechial haemorrhage, caused by head rotation as in some sporting, scooter and automobile accidents; and 5 percent had epidural haematoma (EDH), often seen in sports injuries such as being hit with a baseball.
Average age of the patients was 41 and 66 percent were male. They were followed-up at two weeks, and at three-, six- and 12 months following injury. Patients in the SAH/SDH/contusion group failed to make a complete recovery at 12 months post-injury and had a range of outcome impairments, from mild to more severe.
Patients in the IVH/petechial haemorrhage group tended toward more severe impairments, in the lower-moderate disability range, a level potentially affecting multiple areas of function, such as employment, social and leisure activities, up to 12 months post-injury. Patients with EDH fared significantly better and demonstrated complete recovery by their six-month assessment.
Results from CENTER-TBI, a parallel brain injury research group that had enrolled 2594 participants at European trauma centres. validated the findings. “The confirmation of the findings in an independent cohort confirms the fidelity of our results,” said Manley, adding that patients with EDH were one exception, with incomplete recovery lingering for months longer than those patients followed by TRACK-TBI. However, more severe outcomes were not seen at any point in either study.
The researchers noted that even among concussion patients with positive CT scans, only 39 percent get follow-up care, which should be routine. They also cautioned that their findings are not a call for increased CT use, which has radiation dose concerns and is restricted to known or suspected concussions.
Indeed, a recently approved rapid hand-held blood test may reduce the amount of CT scans. Manley found this test was more sensitive than CT in detecting concussion. The blood test measures biomarkers associated with TBI, which were nearly 52 times higher in MRI-identified concussion patients than in healthy participants.
In addition to challenging the belief that CT features in concussion are not relevant, the researchers are also challenging the idea that concussion is “what the patient brings to the injury,” said Manley, who is also affiliated with the UCSF Weill Institute for Neurosciences. “In moderate and severe TBI, it is anecdotally taught that outcome is determined by ‘what the injury brings to the patient,’ while concussion is determined by baseline characteristics like age, sex and years of education. While the study confirms the importance of these characteristics, we show that in some concussion cases, poor outcomes are also attributed to ‘what the injury brings to the patient.'”
Source: University of California, San Francisco
Journal information: Yuh EL et al., Pathological computed tomography features associated with adverse outcomes after mild traumatic brain injury, JAMA Neurology, July 19, 2021.