Phase 1 Clinical Trial of a Gene Therapy for Alzheimer’s

Researchers at University of California San Diego School of Medicine have received a grant to conduct a first-in-human Phase 1 clinical trial of a gene therapy for treating Alzheimer’s disease (AD) or Mild Cognitive Impairment (MCI), a condition often preceding dementia.
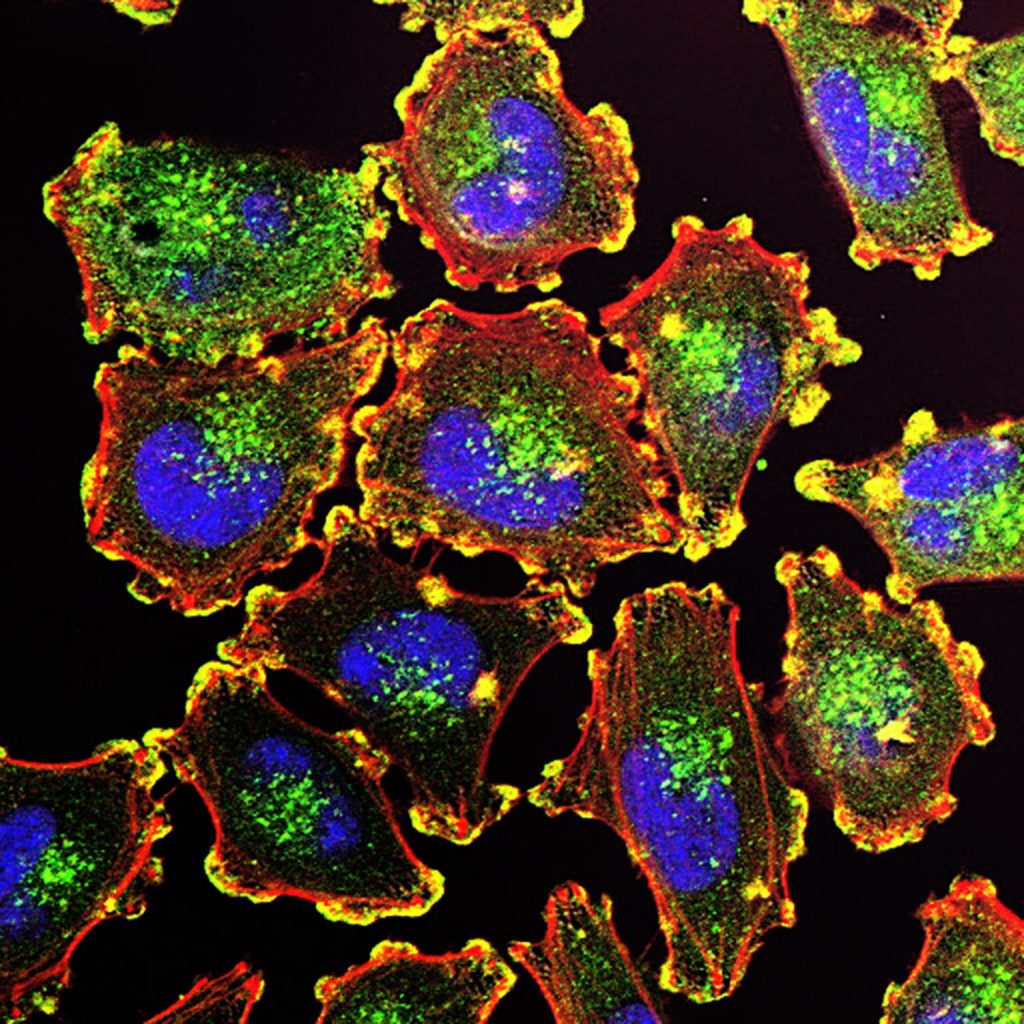
Gene therapy is an experimental technique that uses genes or gene products for the treatment or prevention of diseases by altering the DNA of living cells. Viral vectors are commonly used to insert the DNA changes into the target cells’ nuclei, but non-viral vectors also exist though they are generally less efficient.
The clinical trial, developed by principal investigator Mark Tuszynski, MD, PhD, professor of neuroscience and director of the Translational Neuroscience Institute at UC San Diego School of Medicine, delivers the brain-derived neurotrophic factor (BDNF) gene into the brains of qualifying trial participants where it is hoped it will stimulate BDNF production in cells.
BDNF belongs to a family of growth factors (proteins) found in the brain and central nervous system that support existing neurons and promote growth and differentiation of new neurons and synapses. BDNF is particularly important in brain regions susceptible to degeneration in AD.
“We found in earlier studies that delivering BDNF to the part of the brain that is affected earliest in Alzheimer’s disease — the entorhinal cortex and hippocampus — was able to reverse the loss of connections and to protect from ongoing cell degeneration,” said Tuszynski. “These benefits were observed in aged rats, aged monkeys and amyloid mice.”
The three-year-long trial seeks to recruit 12 participants with either diagnosed AD or MCI to receive AAV2-BDNF treatment, with another 12 persons serving as a control group over that period.
This will be the first safety and efficacy assessment of AAV2-BDNF in humans. A previous gene therapy trial from 2001 to 2012 using AAV2 and a different protein called nerve growth factor (NGF) found increased growth, axonal sprouting and activation of functional markers in the brains of participants.
“The BDNF gene therapy trial in AD represents an advance over the earlier NGF trial,” said Tuszynski. “BDNF is a more potent growth factor than NGF for neural circuits that degenerate in AD. In addition, new methods for delivering BDNF will more effectively deliver and distribute it into the entorhinal cortex and hippocampus.”
Source: UC San Diego