Dengue Linked to Heightened Short- and Long-term Risk of Depression in Taiwan
New study also uncovers short-term links with sleep disorders

Analysis of the medical records of nearly 50 000 people who experienced dengue fever in Taiwan suggests that this disease is associated with elevated short- and long-term risk of depression. Hsin-I Shih and colleagues of National Cheng Kung University and National Health Research Institutes, Taiwan present these findings in the open-access journal PLOS Neglected Tropical Diseases.
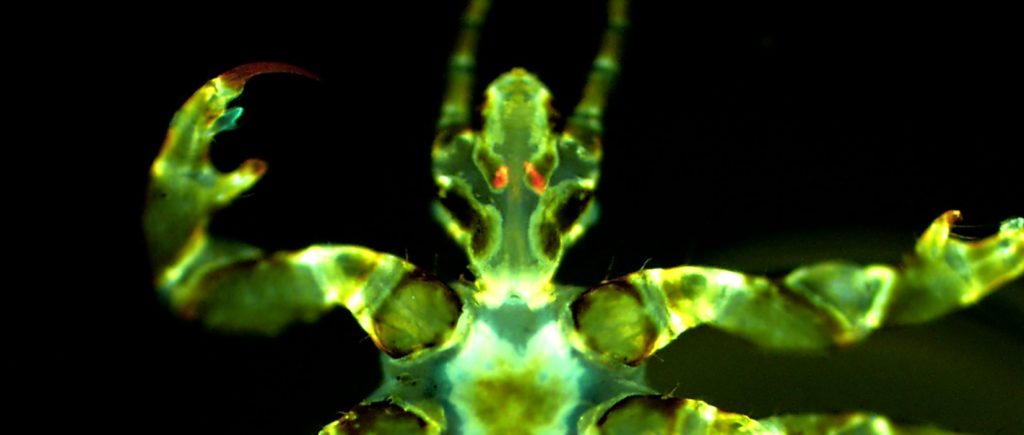
People may develop dengue fever after being bitten by a mosquito carrying the dengue virus. Dengue fever can be mild, but it can also progress to life-threatening severity, and some people may have long-term health effects. Prior research has uncovered links between active dengue fever and psychiatric disorders, such as depression and anxiety. However, few studies have examined the long-term risk of such disorders after a dengue infection.
To address this knowledge gap, Shih and colleagues analysed the medical records of 45 334 dengue patients in Taiwan and, for comparison, 226 670 patients who did not experience dengue. Covering the years 2002 to 2015, the researchers examined whether dengue patients were more likely to develop anxiety, depressive disorders, and sleep disorders at various time points after infection. To help account for other factors that could influence mental health, the dengue patients were grouped with demographically similar non-dengue patients for statistical analysis.
The researchers found that the dengue patients had a greater likelihood of developing a depressive order across all timeframes, including less than three months, three to 12 months, and more than 12 months after their infection. Sleep disorders were only elevated within three to 12 months post-infection, and there was no observable elevated risk of anxiety.
Taking a closer look at patients whose dengue was severe enough for them to be hospitalized, the researchers found an elevated risk of anxiety disorders within the first three months of infection, as well as elevated risk of sleep disorders in the first 12 months. This subgroup also had elevated risk of depression across timeframes.
These findings suggest a potential link between dengue fever and subsequent depressive disorder. However, further research is needed to determine whether dengue contributes directly to development of depression, or if the association is due to some indirect mechanism.
The authors add: “This study highlights a significant association between dengue fever and an elevated risk of depression in both the short and long term, underscoring the need for further research into the mental health impacts of dengue infection.”
Provided by PLOS