Tofacitinib Could Treat Rare but Deadly Systemic Sclerosis

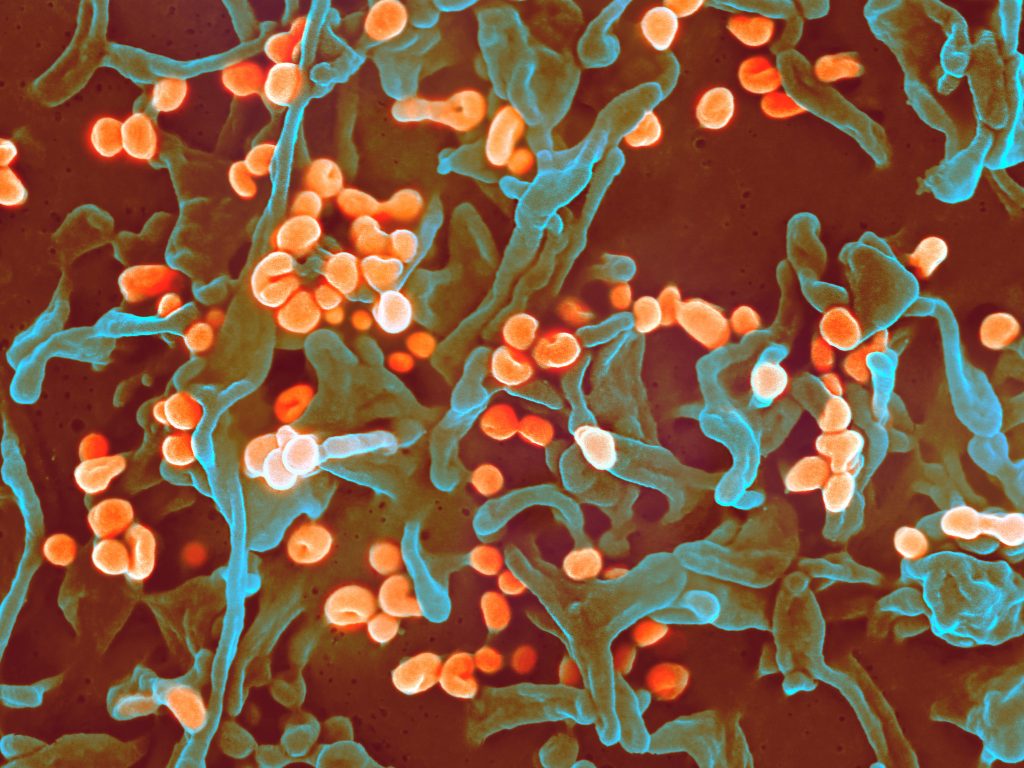
Systemic sclerosis, or scleroderma that affects the skin and internal organs, is one of the rarest autoimmune diseases, affecting roughly 100 000 people in the US, mostly women. It has the highest mortality rate among rheumatic diseases.
There are no licensed treatments available for this subset of scleroderma patients, and rheumatology researchers are constantly searching for opportunities to use resources and technology that have proven beneficial in treating other autoimmune and rheumatic diseases.
In a new study published in JCI Insight, researchers found that tofacitinib, a drug approved for rheumatoid arthritis, was well tolerated among patients with early systemic sclerosis, and discovered the drug primarily affected the protein, interferon, both in fibroblasts and keratinocytes cells.
Dinesh Khanna MBBS., MSc, director of the Michigan Medicine Scleroderma Program, explained: “We wanted to understand first, if there was any clinical benefit of tofacitinib to patients, but we were also asking, what are the differences in the cells of healthy skin versus systemic sclerosis cells…how does the drug work?”
The study sample size consisted of 15 patients with early diffuse cutaneous systemic sclerosis — patients with skin hardening and issues with organs. Of the total participants, 10 patients received 5mg of tofacitinib twice a day, and the remaining received placebo in a double-blind randomised placebo-controlled trial.
Over the course of the 24-week trial period, researchers found no patients who exhibited severe adverse effects at or before the trial ended. Measures included the modified Rodnan skin score (mRSS).
These results showed that the average mRSS score and other measures improved over the course of the trial. In addition, patients on placebo went on open label tofacitinib after 24 weeks and there was ongoing improvement during the next 24 weeks, indicating improvement in the measure.
“We are delighted to find that the drug is safe to use and can possibly be repurposed for systemic sclerosis treatment,” said Khanna, “but what made this study innovative was the use of single cell technology.”
Participants in the study had a skin biopsy at the start of the trial and then again six weeks after they received tofacitinib or placebo. Then, clinicians used the relatively new technology — single cell RNA sequencing — to watch the mechanism of tofacitinib at work in the trial participants’ skin cells.
“This work highlights the ability of single-cell RNA-sequencing to determine how disease states are maintained and how various cell populations in the skin, both fibroblasts, skin cells, and immune cells communicate, providing unparallelled power to address disease mechanisms, and how drugs, like tofacitinib, work in a disease where they have not previously been used,” said Johann Gudjonsson MD, PhD, professor of dermatology and a collaborator on this study.
Along with discovering how tofacitinib inhibits fibroblasts and keratinocytes, researchers found that the drug had minimal effect on T cells.
“Because we found that the drug was working on one part (the mechanism of fibroblasts and keratinocytes), we are now considering if we can combine tofacitinib with another drug with complementary mechanism in action, in order to treat early systemic sclerosis without causing toxicity,” explained Khanna.
To understand more about the drug, researchers will need to conduct a more robust study and trial to see if their recent discoveries hold true.
“From this combined effort between Michigan Medicine and University of Pittsburgh, we know that the drug is safe, and we know that the technology (RNA sequencing) is feasible, now we can start to utilise the technology and find out what type of therapies we can mix and match that will add benefit to patients,” Khanna said.