Dermatology Researchers Discover New Skin Disease with Innovative Approach
In a recent paper published in Scientific Reports, researchers from the University of Maryland School of Medicine described a new skin disease in a male patient with erythroderma, causing 80% of his skin to be covered with red, exfoliating skin lesions that itched and burned. After undergoing months of treatment with traditional therapies for erythroderma, which included the steroid prednisone, anti-itch creams, and immunosuppressive drugs, the patient experienced little relief.
“We isolated individual circulating blood cells and created a new blood test using flow cytometry to identify specific cytokine signatures,” said study corresponding author Shawn Kwatra, MD, the Joseph W. Burnett Endowed Professor and Chair of Dermatology at UMSOM and Chief of Service Dermatology at the University of Maryland Medical Center (UMMC). The authors received a patent for this new method, involving “peripheral blood flow cytometry-based immunophenotyping enabled us to identify a novel form of a severe and potentially life-threatening skin disease.”
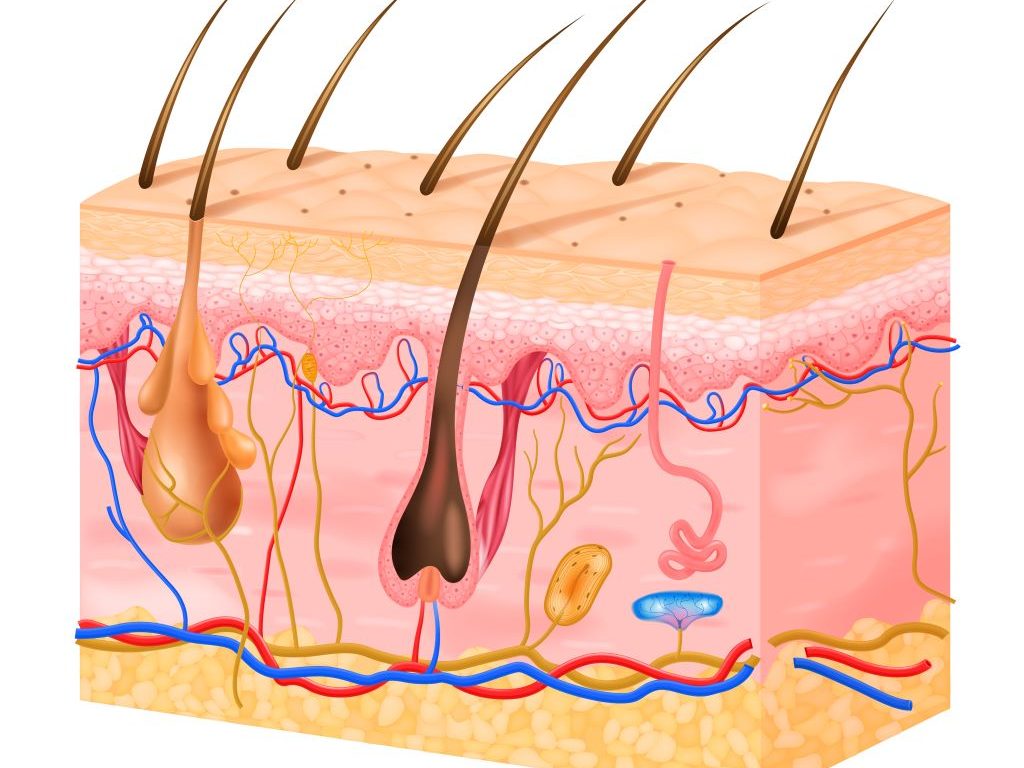
Erythroderma is a rare but severe and potentially life-threatening inflammation that occurs on most of the body’s skin surface. It causes redness and scaling of the skin that spreads over the body and causes the skin to slough off. This can lead to problems with thermoregulation and can cause protein and fluid loss, leading to severe complications.
To determine which of the immune system’s components were driving the inflammatory disease, Dr Kwatra and his team used a new flow cytometry platform technique, for which they received a patent, to immunophenotype skin diseases. They found that two of these cytokines, called interleukin-13 and interleukin-17, were at increased levels in this patient compared to healthy controls as well as when compared to patients with other known causes of erythroderma. Subsequently, targeted treatment with biologic inhibitors of IL-13 and IL-17 reversed the patient’s disease.
“We found a new role for interleukin-13 and interleukin-17 in the blood samples taken from this patient which supported the use of those two particular medications,” said study first author Hannah Cornman, MD, an incoming dermatology resident at the University of North Carolina who conducted the research as a medical student at UMSOM. “These cytokines appeared to be the key cytokines in defining the disease.”
When the patient was treated with a dual therapy of two monoclonal antibodies, dupilumab and secukinumab, his symptoms dramatically decreased and eventually resolved, essentially curing him of his erythroderma. The authors also identified the cell sources of these pathological cytokines and monitored the decline in immunopathogenic (disease-causing) cell numbers, and the decline of interleukin-13, and interleukin-17 levels in the patient’s blood throughout the treatment course.
“We created a new diagnostic test to discover a previously undescribed skin disease and initiate appropriate treatment. We are now exploring developing our diagnostic test to a range of other inflammatory skin,” said Dr Kwatra.









