A Nearly Five-fold Increase in Hospitalisations for Common Cause of Stroke
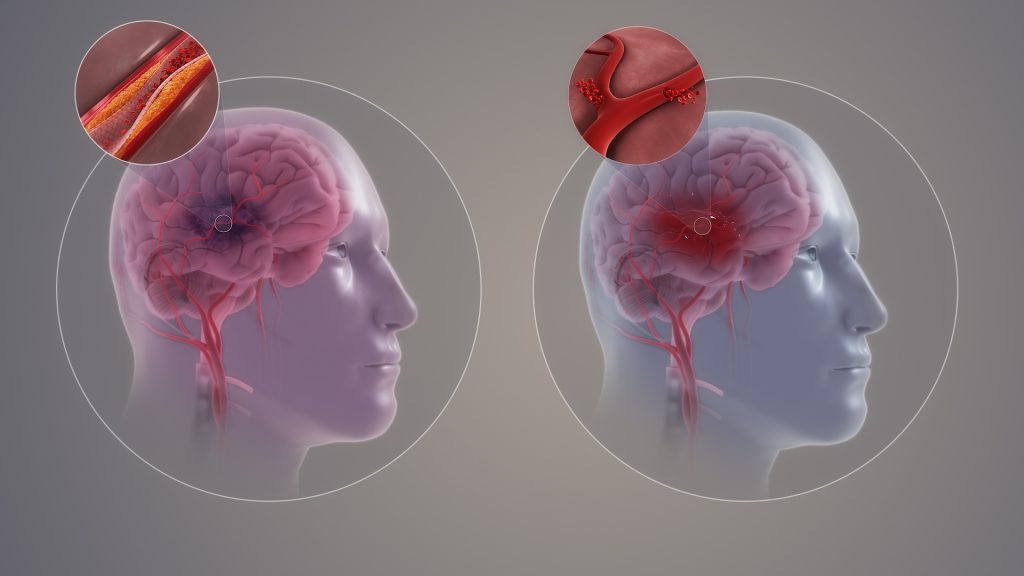
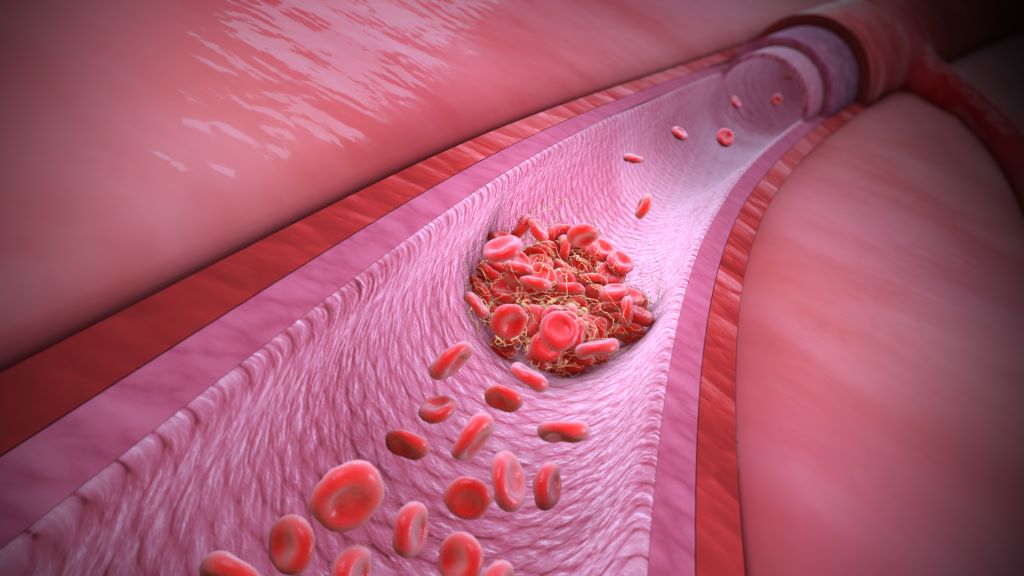
Cervical artery dissection is a tear in an artery in the carotid or vertebral artery, and can result in blood clots that cause stroke. A new study has found almost a five-fold increase in the number of U.S. hospitalisations for cervical artery dissection over a 15-year period. The study is published on April 2, 2025, online in Neurology®, the medical journal of the American Academy of Neurology (AAN).
A dissection in the artery wall is most often caused by trauma due to motor vehicle accidents but can also occur with smaller injuries. Heavy lifting has also been shown to cause dissection in some people.
“Cervical artery dissection is an important cause of stroke, especially in people under 50, so it is crucial to detect it right away,” said Shadi Yaghi, MD, of Brown University in Providence, Rhode Island. “Strokes that are not fatal can lead to long-term disability, poor mental health and reduced quality of life. Our research found a dramatic increase in the number of hospitalisations for cervical artery dissection with rates rising steadily year over year.”
For the study, researchers reviewed 15 years of U.S. health data to identify 125 102 people hospitalised for cervical artery dissection. Participants had an average age of 51, and just over half had a stroke at the same time as dissection. Of all participants, 65% were white, 10% were Black, 8% were Hispanic, 3% were Asian or Pacific Islander, and 14% were of other racial groups. Researchers compared the number of hospitalisations to U.S. Census data to determine the annual rate of cervical artery dissections. They then calculated the average annual percentage change in those rates.
Researchers found the number of dissections increased from 11 cases per one million people in 2005 to 46 cases per one million people in 2019, with an average annual increase of 10%. Results were similar for both female and male participants. The average annual increase for Hispanic participants was 16%; for Black participants it was 13%, Asian participants, 12% and white participants, 8%.
Researchers also found a greater average annual increase among people 65 and older at 12% compared to 8% for people under 65.
“Possible reasons for this nearly five-fold increase over 15 years include greater awareness of cervical artery dissection by health care professionals, better access to imaging to help identify it and an overall increase in this condition for which a cause has yet to be determined,” said Yaghi. “Given the rising incidence of cervical artery dissection, our study underscores the importance of finding prevention strategies as well as new treatments to reduce the risk of stroke.” A limitation of the study was that the hospital admission data does not include undiagnosed or untreated cases, so the number of cases may be even higher.
Source: American Academy of Neurology